Development of the IMB Model and an Evidence-Based Diabetes Self-management Mobile Application
Article information
Abstract
Objectives
This study developed a diabetes self-management mobile application based on the information-motivation-behavioral skills (IMB) model, evidence extracted from clinical practice guidelines, and requirements identified through focus group interviews (FGIs) with diabetes patients.
Methods
We developed a diabetes self-management (DSM) app in accordance with the following four stages of the system development life cycle. The functional and knowledge requirements of the users were extracted through FGIs with 19 diabetes patients. A system diagram, data models, a database, an algorithm, screens, and menus were designed. An Android app and server with an SSL protocol were developed. The DSM app algorithm and heuristics, as well as the usability of the DSM app were evaluated, and then the DSM app was modified based on heuristics and usability evaluation.
Results
A total of 11 requirement themes were identified through the FGIs. Sixteen functions and 49 knowledge rules were extracted. The system diagram consisted of a client part and server part, 78 data models, a database with 10 tables, an algorithm, and a menu structure with 6 main menus, and 40 user screens were developed. The DSM app was Android version 4.4 or higher for Bluetooth connectivity. The proficiency and efficiency scores of the algorithm were 90.96% and 92.39%, respectively. Fifteen issues were revealed through the heuristic evaluation, and the app was modified to address three of these issues. It was also modified to address five comments received by the researchers through the usability evaluation.
Conclusions
The DSM app was developed based on behavioral change theory through IMB models. It was designed to be evidence-based, user-centered, and effective. It remains necessary to fully evaluate the effect of the DSM app on the DSM behavior changes of diabetes patients.
I. Introduction
The utilization of mobile technologies to deliver healthcare services anytime, anywhere has increased in recent years [1]. A report by the World Health Organization in 2012 stated that mobile healthcare will help address the shortage of healthcare resources and thus improve the healthcare services provided to the population [2]. Among various mobile healthcare services, there has been an increase in the use of smartphone sensors for lifestyle monitoring, which has included the self-management of patients with chronic diseases [3].
In addition to oral medication or insulin therapy, diabetes self-management (DSM) involving the management of lifestyle factors, such as diet and exercise, significantly affects the prognosis of diabetes mellitus [4]. Smartphones have been actively applied to DSM behaviors, such as diet, exercise, and medication management. According to a healthcare report by Intercontinental Marketing Services (IMS) Health published in 2015, DSM mobile applications (apps) were the second most common type of chronic disease management apps (constituting 15% of them) [5]. The systematic literature review of Liang et al. [6] revealed that DSM apps that enable users to manage their lifestyle anywhere, anytime are effective at reducing blood glucose levels.
However, explaining how DSM apps can reduce blood glucose remains elusive because these apps were not developed based on a theoretical framework that underlies the process of behavioral changes [7]. The literature review performed by Riley et al. [8] of 16 DSM apps developed based on behavioral change theory found that only one of them had been developed based on social cognitive theory [9]. However, that DSM app only emphasized self-efficacy, which made it impossible to describe changes in DSM behaviors in a comprehensive manner [10].
The American Association of Diabetes Educators (AADE) selected the information-motivation-behavioral skills (IMB) model with an information factor to assess the effectiveness of diabetes education, a motivational factor to evaluate cognitive changes, and a behavioral skills factor to evaluate the self-efficacy of DSM behaviors [1112]. The IMB model was developed for AIDS prevention behavior by Fisher et al. [11]. According to the IMB model, the performance of health-promotion behavior is supported by being well-informed about the behavior, highly motivated to perform the behavior in both personal and social aspects, and having the appropriate skills to perform the behavior [11]. The effectiveness of the IMB model in diabetes management has been studied in patients with type 1 and type 2 diabetes in the United States [13] and China [14], and in Korean patients with type 2 diabetes [15].
To prevent DSM apps from harming patients, it is important to develop them based on evidence in clinical practice guidelines. Evidence-based interventions can significantly help patients with chronic diseases to develop self-management skills and adopt behaviors to effectively manage their conditions [16]. According to a systematic review of DSM apps by Chomutare et al. [17], even though most DSM apps are consistent with recommendations in clinical practice guidelines, only 20% of these apps provide tailored interventions that reflect the DSM knowledge and behaviors of individual patients. It is more effective to provide care based on individual needs and preferences, so evidence-based tailored interventions need to be developed [18].
To maximize the effectiveness of DSM apps, it is important for them to provide reminders and social support as well as a communicating function with healthcare providers, in addition to lifestyle management, medication management, and tailored interventions [17]. However, no previously developed app provides all of the following functions in an integrated manner: personalized education, reminders, social media, and interfacing with a glucometer [617]. Chomutare et al. [17] proposed DSM apps with the following functions: insulin and medication management, communication with healthcare providers, dietary management, exercise management, weight management, blood pressure management, linkage to electronic medical records, personalized education based on clinical practice guidelines, social media for social support, and a reminder function.
To encourage patients to use DSM apps continuously, these apps should be developed based on user preferences. Previous studies of DSM apps have shown positive results for blood glucose control [6]; however, the failure rates have been high, and the uptake rate has been low due to usability issues [19]. LeRouge and Wickramasinghe [19] reported that only 18 DSM apps had a user-centered design. The focus group interview (FGI) is the most frequently used qualitative research method for identifying user requirements in both detail and depth. Therefore, based on the IMB model (which systematically explains the changes in DSM behaviors) and evidence extracted from clinical practice guidelines, it is necessary to develop and evaluate a DSM app that implements the functions extracted from a literature review and identified through FGIs with diabetes patients.
II. Methods
We developed and evaluated a DSM app that provides evidence-based personalized education, reminders, an online community for users to interact with other patients, and an interface with a glucometer. We developed the app in accordance with the following four stages of the system development life cycle: analysis, design, implementation, and evaluation (Figure 1).

The application was developed in accordance with the following four stages of the system development life cycle: analysis, design, implementation, and evaluation.
1. System Analysis
The functional and knowledge requirements of the users of a DSM app were identified through FGIs with diabetes patients. These aspects were then also extracted from a literature review and validated by experts.
1) Needs assessment
The eligibility requirements for participating in the FGIs included having diabetes, being an adult, and having a smartphone capable of running apps. Participants were recruited through an advertisement posted on the website of a self-help online cafe for diabetes patients from May 11 to 17, 2016. The 19 recruited diabetes patients were divided into two groups. Two nurses interviewed each group for about 1 hour with the aid of the semi-structured questions used in the study of Choi et al. [15].
All of the interviews were recorded and then analyzed using the following qualitative content analysis procedure [20]. First, the audio-recorded FGIs were transcribed verbatim by the first author. A PhD student in nursing who is an expert in qualitative research reviewed the transcripts to check for any missing information. Second, three members of the research team independently developed an initial codebook of themes that arose after an FGI had been conducted and all of the FGI transcripts had been read. The rule applied for the extraction of themes was that the narratives were expressed by at least one FGI participant and could be implemented in the app. Third, the same members reviewed and had periodic discussions to achieve a consensus about the codes to be used and to identify convergent, salient, and/or unique themes. Fourth, the same members then classified all the themes according to the four-category schema (information, personal motivation, social motivation, and behavioral skills) developed by Choi et al. [15]. The final codebook of themes and categories was then reviewed by the PhD student.
2) Functional definition
Functions were extracted based on the functional requirements of users and literature about the implementation of DSM apps. The functional requirements of users were determined by reviewing previous DSM intervention studies, and additional functions were extracted by three nursing informatics experts based on a healthcare report from IMS Health and the systematic review of Chomutare et al. [17].
3) Knowledge extraction
The knowledge provided in the DSM app was extracted from clinical practice guidelines. Two diabetes nurse educators (with 2 years and >10 years of experience) advised the first author about selecting appropriate guidelines and extracting DSM knowledge.
The DSM knowledge was extracted based on the DSM key areas of the AADE excluding psychosocial areas: healthy eating, being active, self-monitoring of blood glucose (SMBG), taking medication, problem-solving, and reducing risks. The extracted knowledge was organized as an assessment of the DSM knowledge and previous behaviors of a patient based on goal setting (setting a realistic goal), feedback (commenting on goal achievements), and evaluation (evaluating the DSM behaviors of the patient).
2. System Design
The design step involved designing a system diagram, data models and a database, an algorithm, and screens and menus, as described below.
1) System diagram
To implement the knowledge and functional requirements extracted from the analysis stage, we designed the overall system diagram. The DSM app consists of a client part running on the user's smartphone and a server part running on the system. We depicted the flow of data between the client and the server. We have drawn the system diagram using Microsoft Office Power Point program.
2) Data model and database
A data model is an abstract model that organizes elements of data and defines the relationships between entities and the relationships to properties [21]. In this study, we defined all the data entities necessary for the DSM app. These data entities each had a data type (such as Boolean, Integer, Date time, Coded text), possible values, and a unit. For example, for a body mass index (BMI) data entity, the data type is float, unit kg/m2, and possible values from 10 to 100. A database was designed to collect data entered by the user in the DSM app, such as blood glucose, diet, exercise, and diary. We used the Erwin software to draw an entity-relationship diagram.
3) Algorithm
An algorithm is an ordered sequence of steps that describe solutions of problems. In this study, algorithms for collecting patient information at the first visit, setting goals, providing DSM education, and evaluating DSM behavior on return visits were developed. We used the free online diagram software (draw.io) to design a flow chart of the algorithms.
4) Screens and menus
The display screens were designed to maximize the convenience and concentration of users during their interactions with the DSM app. The menu was designed to minimize the need to move between screens of the DSM app. The display screens and menus were drafted by the authors and finalized after several rounds of meetings with the designer.
3. System Implementation
The authors planned the DSM app with system diagram, database, algorithms, and screens, and the computer programmer developed the system. The DSM app was developed using Android Studio 2.0 and Java Development Kit 7.0, which are standard Android development environments provided by Google. The server was implemented based on Linux and SQLite, which is supported in the Android development environment. The secure socket layer (SSL) protocol was used so that user information could be transferred securely from the app to the server.
4. System Evaluation
The algorithms and heuristics of the DSM app were evaluated, and a usability evaluation was performed.
1) Algorithm evaluation
The recommendations selected by two diabetes nurse educators and provided by the DSM app were compared using 13 scenarios that were developed by the first author to evaluate the algorithms. The scenarios used in the evaluation included at least one decision-making node from the decisionmaking process for the DSM app. The professional diabetes nurses read each scenario and selected appropriate recommendations based on clinical practice guidelines. The data included the same scenarios that the nurses used and were entered into the DSM app, and then the recommendations from the app were recorded.
A score of +1 was assigned when both the category and details of the recommendations from the DSM app and the diabetes nurses matched. A score of 0 was assigned when the two recommendations were in the same category but with different details, whereas a score of −1 was assigned when the recommendation categories differed. The proficiency and efficiency scores were calculated as follows [22]:

The above equations indicate that proficiency was the ratio of the sum of consistent, partially consistent, and inconsistent recommendations from experts and the app to the total number of recommendations, while the efficiency was the ratio of consistent recommendations from experts and the app to the total number of recommendations.
2) Heuristics evaluation
The heuristics of the DSM app was evaluated using a mobile heuristics tool by two experts with majors in nursing informatics and one expert with a major in medical informatics, each of whom had more than 5 years of experience in his or her field. The following eight principles of Bertini's mobile heuristics tool was measured on a 5-point Likert scale (0 ‘no heuristic problem’ to 4 ‘heuristic problem exists and must be fixed’): visibility of app status, match between the app and the real world, consistency and mapping of the app, ergonomic and minimalist design, ease of input and readability, flexibility and efficiency of personalization, aesthetics and privacy, and realistic error management [23].
Three experts were provided with Android smartphones running the DSM app for 1 day to use and evaluate the heuristics problem and severity scores. When at least two experts raised the same heuristics problem or only one expert did this but the severity score was greater than 4, the app was modified appropriately [23].
3) Usability evaluation
The usability of the DSM app was evaluated by diabetes patients who agreed to participate. We recruited the participants from an online diabetes self-help group. These patients used the diverse functions of the DSM app, such as blood glucose input, diet and exercise input, bulletin board, and interfacing glucometer, for 2 weeks. They received a text message once a week to encourage use of the DSM app. After 2 weeks, we surveyed the users about their experience and satisfaction through an open questionnaire about the blood glucose input function, diet and exercise input function, and feedback function as well as their overall satisfaction with the DSM app.
4) Modification of the DSM app
The comments from the heuristics evaluation and usability evaluation were used to modify the app after it had been reviewed by the three nursing informatics experts.
III. Results
1. System Analysis
1) Needs assessment
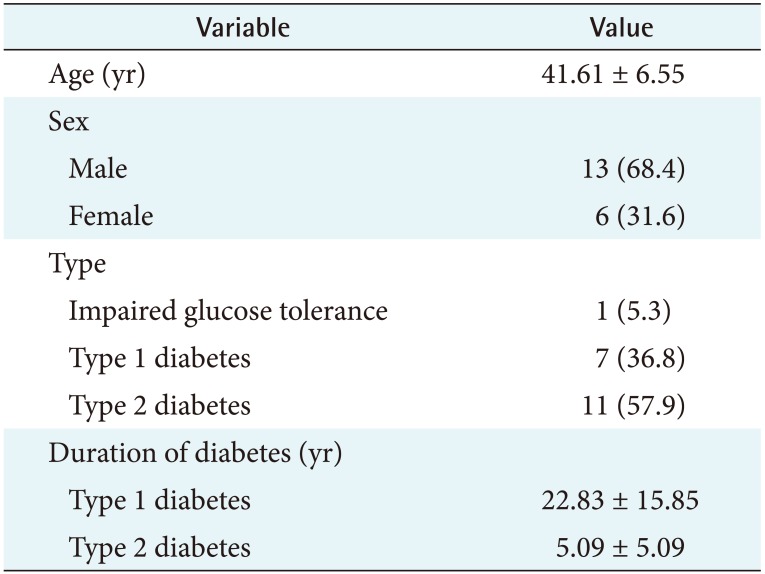
Table 1 presents the demographic characteristics of the FGI participants. These participants were aged between 33 and 55 years (mean, 41.61 years), and more than half of them (68.4%) were male. Seven participants had type 1 diabetes (36.8%), 11 had type 2 diabetes (57.9%), and 1 had impaired glucose tolerance (5.3%). The mean duration of diabetes was 22.8 years in those with type 1 diabetes and 5.1 years in those with type 2 diabetes.
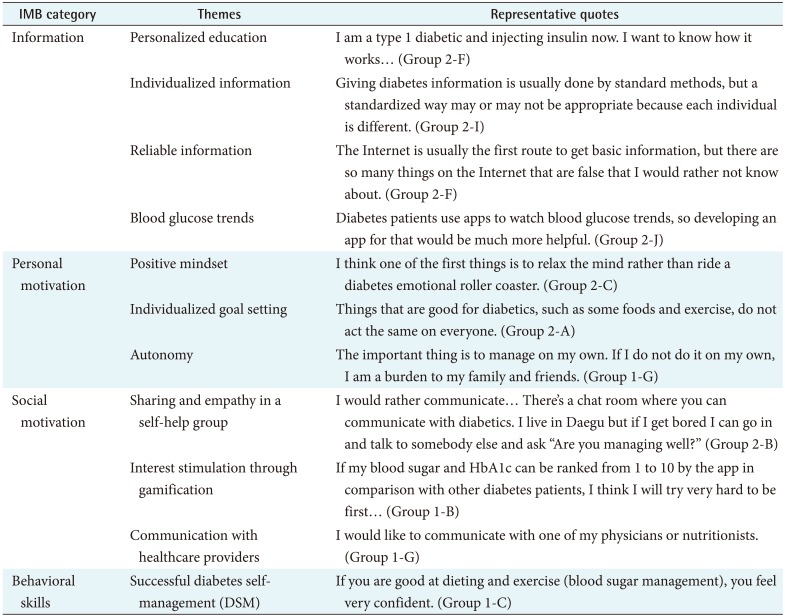
Table 2 presents the categories, themes, and some representative quotes from the focus groups. The 11 themes extracted from the FGIs were organized into the following 4 categories developed from the IMB model:
Information, comprising themes of personalized education, individualized information, reliable information, and blood glucose trends.
Personal motivation, comprising themes of positive mindset, individualized goal setting, and autonomy.
Social motivation, comprising themes of sharing and empathy in a self-help group, interest stimulation through gamification, and communication with healthcare providers.
Behavioral skills, comprising the theme of successful DSM.
2) Functional definition
Sixteen DSM app functions were extracted (Figure 2).

Sixteen diabetes self-management (DSM) app functions were extracted.
IMS: Intercontinental Marketing Services, FGI: focus group interview.
Ten functions (education, recommendations, feedback, setting a goal, recording, checking, diary, sharing, communication, and viewing) were extracted based on the requirements of users from the FGIs. The gamification requirement was not translated into a function because its implementation would require excessive economic and human resources. Two functions for reminding and alerting were extracted from the report of IMS Health [5], one function for the glucometer interface was extracted from Chomutare et al. [17], and three functions for managing the app (registering, login, and notices) were added.
3) Knowledge requirements
The knowledge sources selected included four clinical practice guidelines published by the AADE [4], the American Diabetes Association (ADA) [24], the Korean Diabetes Association (KDA) [25], and Korean Association Diabetes Nurse Education (KADNE) [26]; a relevant paper on DSM published by the Diabetes Education Center of Seoul National University Hospital [27]; the Diabetes Knowledge Test of the Michigan Diabetes Research Center [28]; the DSM assessment report tool (D-SMART) [29], and the food and exercise calorie database of the Korea Food and Drug Administration (KFDA) [30].
The following 49 knowledge rules for DSM were extracted based on the DSM key areas of the AADE: 10 rules for diet, comprising 6 on assessment, 1 on goal setting, 2 on feedback, and 1 on evaluation; 7 rules for exercise, comprising 2 on assessment, 1 on goal setting, 2 on feedback, and 2 on evaluation; 9 rules for SMBG, comprising 4 on assessment, 2 on goal setting, 2 on feedback, and 1 on evaluation; 3 rules for medication adherence, comprising 2 on assessment and 1 on evaluation; 9 rules for reducing risks, comprising 2 on assessment, 3 on goal setting, and 4 on feedback; and 11 rules for problem-solving, comprising 8 on assessment and 3 on evaluation.
Knowledge in the SMBG domain may be illustrated by the following examples. If a patient measures his or her blood glucose less than once a week, the DSM app provides a recommendation about the importance of measuring blood glucose (assessment). If a patient sets a pre-meal blood glucose target below 70 mg/dL, the DSM app provides a recommendation about the appropriate blood glucose target range (goal setting). If a patient achieves the goal, the DSM app provides positive feedback, such as “You have a good blood sugar. Keep your status steady” (feedback). If a patient measures his or her blood glucose less than four times a week or if fewer than half of the recorded blood glucose values are within the normal range, the DSM app provides recommendations about the importance of measuring blood glucose, its normal range, and how to measure it.
2. System Design
1) System diagram
The DSM app consists of two parts (Figure 3), a client part that runs on the user's smartphone and a server part for sharing data with other users. The client part provides personalized education and recommendations based on the user's personal information, health-related information, medication history, and DSM knowledge and performance level. It receives blood glucose levels wirelessly from a glucometer and provides feedback based on individual goals, records of DSM behaviors, and blood glucose levels.
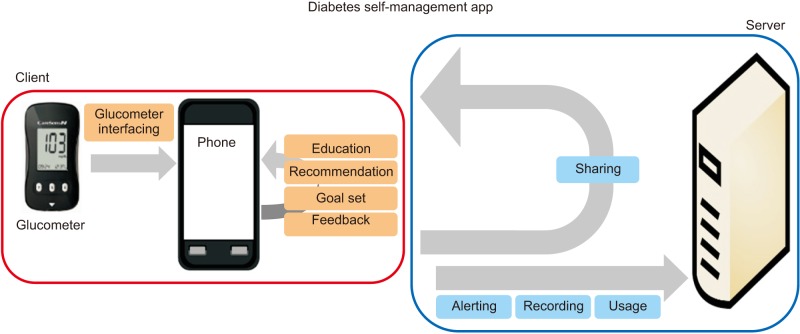
The diabetes self-management app consists of two parts: a client part that runs on the user's smartphone and a server part for sharing data with other users.
The server part has a bulletin board for sharing records with other users and expressing empathy using a ‘like’ button. The record of a user's DSM behaviors, alarm setting, and app access history are collected to the server from the client part after 4 weeks of app usage.
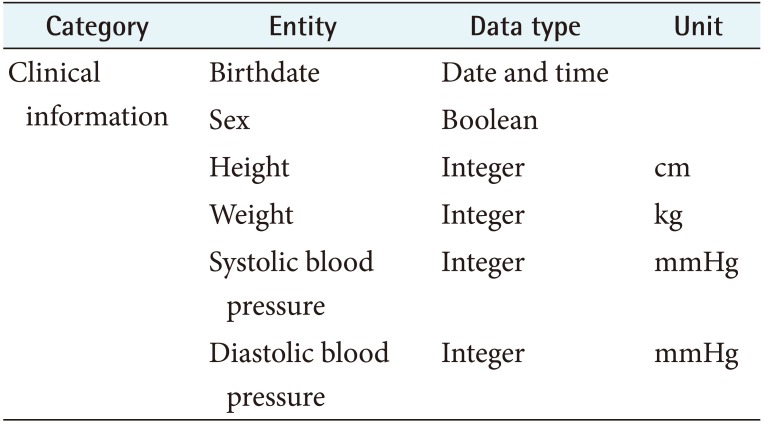
2) Data model and database
The data used in the DSM app were 78 grouped into the following 15 categories: personal information, health-related information, medication history, goal setting, dietary record, food list, exercise record, exercise list, diary, blood glucose, medication compliance, blood pressure and weight, foot care, evaluation rules, and overall. Data models were created for the 78 data entities with possible values, data types, and units. One of the data models is presented in Table 3.
The database consists of 10 tables without any identifiable data elements in order to minimize security problems. A primary key was created by combining the registration time, email address, and a nickname, rather than using identifiable data elements. The 10 tables comprise personal information, dietary records, food list, exercise record, exercise list, blood glucose, medication adherence, blood pressure and weight, foot care, and an alarm.
3) Algorithm
The DSM app algorithm shown in Figure 4 was developed based on the functions and knowledge extracted in the analysis step.

The diabetes self-management app algorithm was developed based on the functions and knowledge extracted in the analysis step.
The patients who used the DSM app for the first time were asked to complete consent forms. Their personal information, health-related information, medication history, and DSM performance level were assessed (box A in Figure 4). Next, the patients set their goal, that is, amount and periods of DSM behaviors. If a goal was assessed by the system as unrealistic, more-appropriate values for the amount and period of DSM behaviors based on clinical practice guidelines were recommended in a pop-up window (box B in Figure 4).
After setting a goal, the patient's knowledge level of DSM behaviors was assessed, and the app provided personalized education according to this level of knowledge (box C in Figure 4). For example, a patient who did not select the correct answer (“one glass of diet cola”) in response to the question “what is incorrect hypoglycemic therapy” was considered to be lacking knowledge about how to cope with problems. In such a case, the app would provide personalized education about a “hypoglycemia coping method.”
After providing education, the app assessed the adequacy of the DSM behaviors of the patient and provided appropriate individualized recommendations (box D in Figure 4). For example, patients who had never cared for their feet were considered to have inappropriate foot-care habits, so the app provided individualized information on the “significance of foot care” and “foot-care method.”
In the case of patients who reused the DSM app, the app identified their goals set during their first use and provided them with feedback according to goal achievement (box E in Figure 4). The app then provided individualized information according to the evaluation of record fidelity, exercise, diet, SMBG, percentage of normal blood glucose, and adherence with medication based on the record of DSM behaviors in the app, which was written by the user (box F in Figure 4). For example, if the recorded dietary calorie intake over 1 week was less than 60% of the target intake, the app determined that the dietary habits were incorrect and provided individualized information on “normal weight and daily required calories,” “three general principles of healthy eating,” and lists of replacement foods.
4) Screen and menus
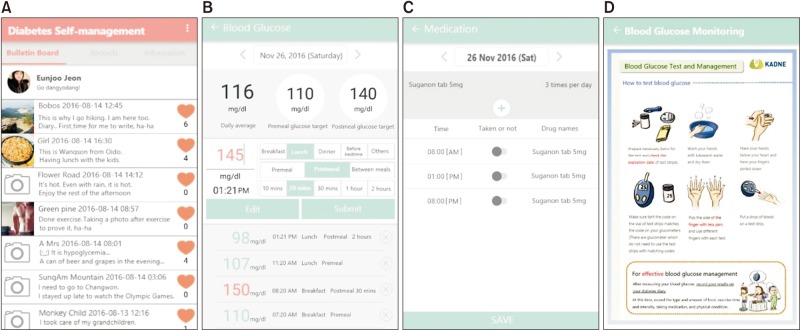
The menu structure of the DSM app comprises 6 main menus: initial input, evaluation, bulletin board, record, information, and option. The initial input menu appears as a pop-up screen when the user accesses the DSM app for the first time, and the evaluation menu appears when the user accesses the DSM app after the set target period has elapsed; thus, it was designed without a submenu. The bulletin board, record, information, and option main menus were designed as fixed menus of the DSM app, and the main menu of the bulletin board was designed as a shared diary submenu. The record main menu consists of profile, diary, blood glucose, diet, exercise, medication, blood pressure and weight, and foot-care submenus. The information main menu consists of SMBG, healthy diet, exercise, medication, problem-solving, daily record view, graph view, and statistical analysis submenus. The option main menu consists of goal setting, reminder, notices, communication, and glucometer-interface submenus.
Forty user screens were designed to implement 6 main menus and 22 submenus in the app. The screen for the bulletin board, SMBG information, medication adherence checking, and blood glucose level recording are shown in Figure 5.
3. System Implementation
The operating environment of the DSM app is Android version 4.4 or higher so that low-power Bluetooth connectivity (version 4.0) is supported. The DSM app was developed from February to May 11, 2016 with the help of a doctoral student in computer science. It was registered as ‘diabetic-diabetes management friend’ in the Google Play Store.
4. System Evaluation
1) Algorithm evaluation
The proficiency of the DSM algorithm was evaluated by two evaluators as 91.43% and 90.48% (mean, 90.96%). The efficiency of the DSM algorithm was evaluated as 94.29% and 90.48% (mean, 92.39%).
The recommendations of the experts and the app did not match for SMBG. The DSM app did not provide SMBG information to users who made measurements at least twice daily, in accordance with the AADE evaluation criterion of at least once daily. However, evaluator A suggested that people who faithfully self-monitor their blood glucose should be consistently provided with SMBG information. SMBG requires more-specialized knowledge than diet and exercise management, so the algorithm was modified to provide SMBG information to users who exhibited good behavior in checking blood glucose.
2) Heuristics evaluation
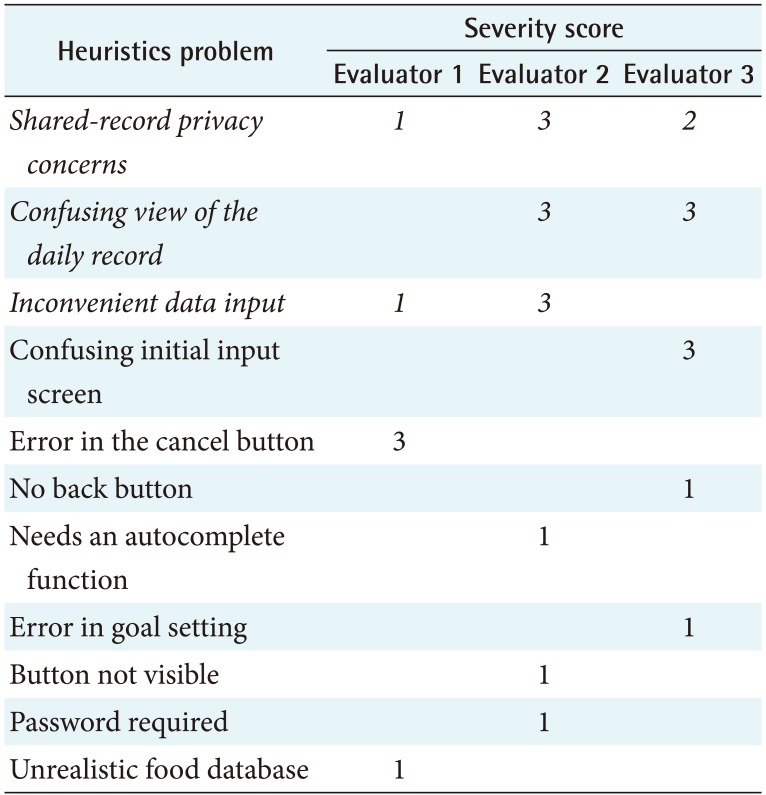
The heuristics evaluation of the DSM app revealed 15 issues (Table 4). The following three issues were considered by at least two evaluators to be serious, so the app was modified accordingly (italicized in Table 4): “since every record is shared, there may be privacy concerns,” “it is difficult to grasp the DSM behaviors in the record view at a glance,” and “it is inconvenient to be required to input the blood glucose level when entering a diet and exercise record.”
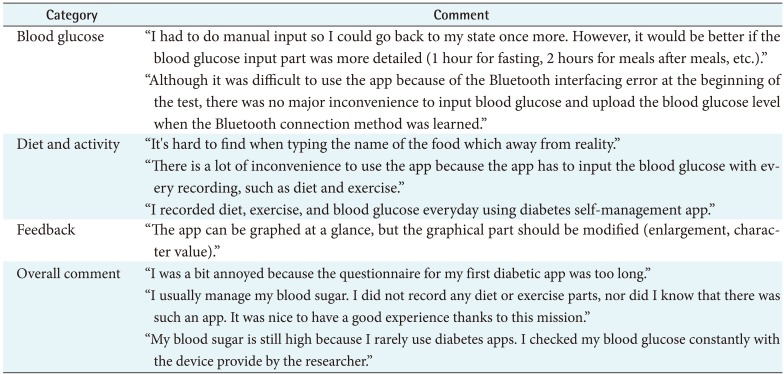
3) Usability evaluation
Usability evaluation was performed with the participation of 14 diabetes patients (8 men, 6 women) with a mean age of 43 years. Five major modifications were proposed (Table 5). They are blood glucose input screen; number of blood glucose inputs; diet, exercise input screen; blood glucose trend graph; and change of food and exercise name.
4) Modification of the DSM app
We modified the DSM app based on the heuristics and usability evaluation. First, we reduced the number of questionnaire items from 100 to 20 and mandatory input items. Second, we removed the limit for the number of blood glucose inputs and modified the blood glucose test time to be more detailed (‘morning’ - ‘before and after’ - ‘10 minutes’ combination). Third, we divided the input window into two for recording and viewing. Fourth, we added a function for users to select the level of record disclosure as “only the author can see” or “share”. Fifth, we upgraded the data visualization of the DSM app, query period, and viewing of blood glucose values. Finally, we modified the food database to provide representative food names and calorie information, including recipes, ingredients, and local food names.
IV. Discussion
The DSM app developed in this study has three characteristics based on behavioral change theory: personalized, evidence-based, and user-centered. To implement these 3 characteristics, 16 functions were integrated into a single DSM app.
1. Behavioral Change Theory-based App
An app-based intervention utilizing specific functionality that is only available on a mobile platform can be more effective than traditional face-to-face diabetes management based on the IMB model. The mobile DSM app provides personalized information regardless of the time and place to increase knowledge (information), gives instant feedback for realistic goal setting (personal motivation), links into a social network with other diabetes patients (social motivation), and provides feedback from healthcare workers regardless of time and place to increase confidence in their self-ability to perform behaviors (behavioral skills) [1317].
The DSM app developed in this study provides personalized education, individual information, reliable data from the KFDA, and blood glucose trends to increase the quality of the information. It encourages writing a diary and setting an individual goal to promote personal motivation and provides a bulletin board for patients to share their individual experiences and empathize with each other to promote social motivation. Further, it provides feedback to the patients to promote their behavioral skills.
2. Personalized and Evidenced-Based Interventions
The AADE published clinical guidelines for diabetes using systematically developed statements based on the best research evidence and recommended the provision of personalized education [4]. Haas et al. [31] also demonstrated that it is effective to provide personalized information based on the DSM behaviors exhibited by a patient.
A systematic review found that many studies using DSM apps provided evidence-based intervention based on guidelines only, with insufficient personalization [17]. Therefore, in the present study, we extracted DSM knowledge based on the clinical practice guidelines from the ADA [24], KDA [25], and KADNE [26], and we used this information to develop an algorithm to provide personalized information. The algorithm in our DSM app assesses a patient's level of DSM knowledge and DSM behaviors, and it uses this information to provide a tailored intervention.
3. User-Centered Design Using FGIs
We confirmed in the evaluation stage whether the usercentered design had been successfully implemented based on FGI results. For example, the function of choosing the measurement time was developed based on users wanting to record the measurement time in detail, such as “30 minutes before breakfast” or “1 hour after lunch”. There was positive feedback about allowing the patients to choose a measurement time, such as “before breakfast” and “after breakfast”, directly for a measured blood glucose value.
In some cases, the user requirements were extracted during the evaluation. For example, there was a request to not limit the maximum number of blood glucose inputs. This is probably due to diabetes patients needing to monitor their blood glucose closely. We modified the DSM app to satisfy this requirement, which elicited favorable user responses.
4. Effective Integration of DSM App Functions
We were able to effectively implement the three above-mentioned characteristics by developing a DSM app that utilizes specific functionality that is available on a mobile platform.
Previous studies have also demonstrated that functions developed in DSM apps can be effective, such as personalized education [431], goal setting [29], recording and tracking of blood glucose [32], diary writing [33], social networking [34], feedback [32], and reminders [35], and interfacing with a glucometer [5]. In this study, the DSM app developed in the present study not only applied these functions that were found to be effective for blood glucose control, but also integrated diverse function types within a single app. Whether the DSM app that integrates these functions is actually effective in diabetes management will need to be confirmed in future experimental studies.
Notwithstanding these advantages, the DSM app used in this study was only developed to run on the Android operating system, so it needs to be expanded to iOS, Windows, and BlackBerry devices. This study did not evaluate whether the DSM app developed in this study improved the self-management behavior of diabetic patients. A future study is needed to evaluate the effect of the DSM app on the improvement of diabetes management behavior in terms of each factor of the IMB model.
We learned several lessons in this study while developing the DSM app. The lessons include minimizing the gap between the diverse needs of diabetic patients and recommendations of diabetes guidelines. Diabetic patients tend to follow myths and folk medicine. The selection of these various requirements based on evidence was the most difficult task. Second, to develop diabetes management mobile apps, researchers have to act as program planners. Researchers need to have some understanding of system development and design, as well as knowledge of diabetes management, and have to actively communicate with planners, developers, and designers. Researchers also have to understand the system development process and manage a development schedule. Researchers who develop healthcare apps should be well prepared for system development, design, and project management.
Acknowledgments
This work was supported by a grant of the National Research Foundation of Korea (NRF) funded by the Korean government (Ministry of Science, Information and Communication Technology and Future Planning) (No. 2010-0028631).
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.