|
 |
- Search
| Healthc Inform Res > Volume 17(2); 2011 > Article |
Abstract
Objectives
To manage a patient's blood pressure and recovery, and to reduce unnecessary hospital visits after heart surgery, we developed and established a telecare service.
Methods
We established and test-operated the system that enabled biometric data to be measured and monitored at home, and directed connections to the video consultation with monitoring personnel and medical staff when abnormal symptoms were detected.
Results
As a result of using the telecare service with patients discharged from the hospital after undergoing heart surgery, the patients were mostly satisfied with the service and use of the equipment, and some patients wanted to actually receive the service continuously along with a device which could be more easily used.
U-health, which is a new medical paradigm involving healthcare and medical services, uses wire and wireless networking, such as remote patient monitoring, and is available anytime and anywhere. U-health means the expansion of medical services in terms of time and space. Recently [1], the concept of medical service has been extended from a single-shot treatment for disease to a lifetime care and the desire to pursue health is increasing, a new model of medical service (at-home telecare service) has emerged.
The telecare service is one type of e-healthcare using the information and communication technology and provides monitoring information on health conditions and health care services from a distance. The principal telecare services include at-home medical examinations, health maintenance and management services, physical condition monitoring, remote monitoring, and emergency services. The telecare service is a tool of future-oriented health care and improvement and enables patients to manage their health by themselves through education [2].
The telecare service, which monitors the patient's condition at home, has been commercialized in the US and Europe since 1990. Recently, the results of a study have shown that among the patients with heart disease, particularly with cardiac insufficiency, the rate of hospitalization and death decreased by approximately 20% through home monitoring with a corresponding increase in the quality of life and a reduction of medical expenses [3]. In addition, the most common disease in the US and European countries is heart disease, and it is expected to gradually increase as the population ages.
Clark et al. [4] reported that according to some research involving remote monitoring in the US, the rate of hospitalization decreased by 21% and the rate of death decreased by 20%, and thus medical expenses were reduced and the quality of life of the users improved. In addition, Delgado-Passler and McCaffrey [5] reported that a remote care program for heart disease patients following hospital discharge could reduce healthcare expenses due to re-hospitalization. In Brownsell's study [6], telecare services showed an overall affirmative influence on the stability and social participation of the aged. Moreover, according to Chaudhry et al. [7], patients' participation in communicating information about their health status on a daily basis had a favorable effect on their health behaviors, including adherence to medical recommendations. Biddiss et al. [8] reported that telecare is increasingly used to remotely monitor long-term conditions such as congestive heart failure and provide interventions based upon the collected data. In order to improve healthcare efficiency, there remains a need for decision support tools to automate this monitoring function and help guide interventions. Also, Carl et al. [9] reported that telecare services seemed to offer a much wider range of possibilities for specific groups. Telecare services meet a large and growing problem in public policy such as the growing number of older people with chronic illnesses, and the increasing difficulty and costs of providing services that meet their needs. At the same time, there is a problem that there may be major health benefits in delaying admission to hospital and in reducing readmissions in clinical service provision.
It is an important financial issue to continuously monitor heart disease patients and reduce the rate of hospitalization and prevent complications. Accordingly, telemedicine and telemonitoring services are regarded as effective ways of making up for the limitations to manage heart disease patients and provide feedback in general medical services.
The purpose of this study is to implement a system which can monitor the patient's basic biometric data at home for a certain period of time after the patient whose blood pressure needs to be carefully monitored discharges from the hospital after surgery involving the aorta and coronary arteries, and to determine the patient's satisfaction and system improvements.
We conducted a survey on the user needs and satisfaction level among 51 ambulatory patients from the cardiology and the thoracic and cardiovascular surgery clinics of G Hospital, a tertiary hospital located in Incheon, by using telecare services through telemonitoring, and verified the system effectiveness.
10 patients who were discharged after undergoing heart surgery at G Hospital, which is a tertiary hospital located in Incheon, served as the subjects for the study. Biometric data such as blood pressure, pulse, electrocardiograms, and cardiac sounds were measured at home. The telecare service was provided in point of the convenience and improved healthcare for the patients.
The study subjects were 10 patients who had undergone heart surgery such as coronary artery bypass grafts (n = 1), artificial heart valve replacement (n = 2), and aortic aneurysm and aortic dissection repairs (n = 7). The service period was 3 months from April to June 2008.
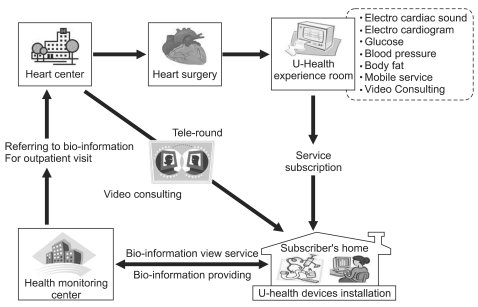
The telecare service has the following components: a personal health device (PHD); a gateway; an application; and a server. In this study, the system is configured as depicted in Figure 1 including two types of devices and an electronic stethoscope.
The data measured at home are transmitted in real-time to the healthcare center of G Hospital and the physician in charge confirms the patient's condition at any time through the EMR system within the hospital or through the web-based management program outside the hospital. A video consultation program is available for real-time consultation. In addition, a mobile service based on the wireless application protocol is available through the physician's mobile phone.
To connect the data measured at home with the EMR system within the hospital, a separate data connection server is necessary. Through the U-health gateway server which plays a role like an aware gateway server, the data transmitted from the gateway within the home is delivered to the information system in the hospital (Figure 2).
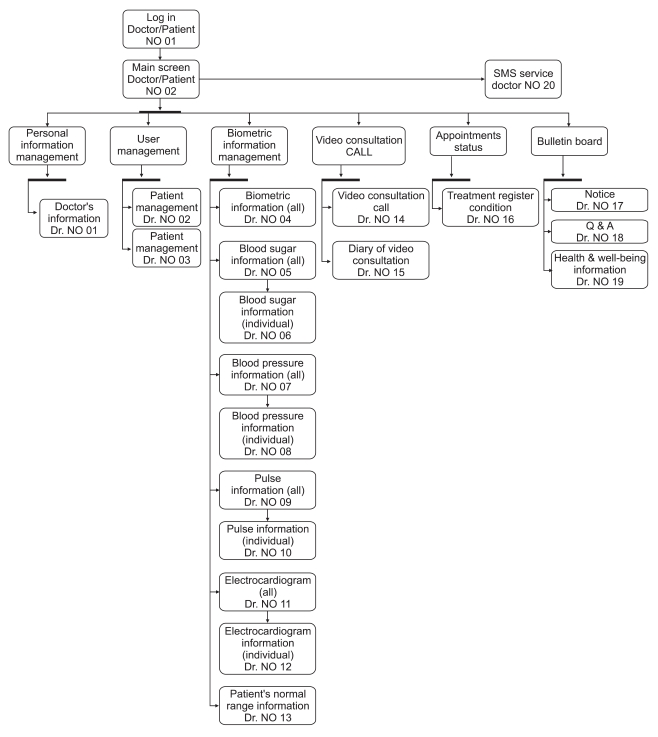
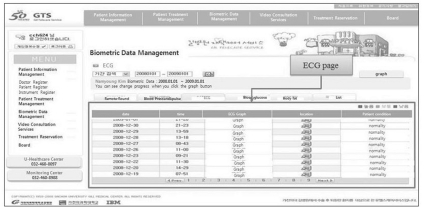
The application comprises a simple user interface (UI) for device measurement and data transmission, and the application model for the physicians is based on the web as shown in Figure 3. The detailed implementation of the user application and the physician application will be addressed in the results.
We installed the devices which can measure biometric data in the user's home and measured the blood pressure, pulse, body fat, cardiac sounds, and electrocardiograms (ECG), and monitored the results in the monitoring center of the hospital.
Based on the biometric data (blood pressure, blood glucose, body fat, physical activity) obtained through the U-health device, the U-healthcare center monitored individual health in connection with the basic information of the examinees.
Furthermore, the telecare service periodically integrated and analyzed the physical information measurement results, and provided a 'newsletter' for the individuals together with other health information.
The blood pressure, pulse, electrocardiograms and cardiac sounds which need be monitored at home after heart surgery were periodically monitored, and in case of need, video conferencing with a physician was available.
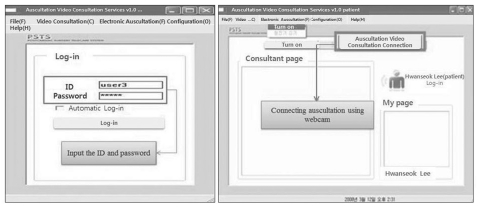
After typing in an user identification (ID) and password registered when joining the service, if the patient logs on and clicks the icon indicating an auscultation video consultation connection, the mark indicating 'connecting with monitoring personnel' appears and after a short interval of time, video consultation with the monitoring personnel occurs.
The measurements of blood pressure, pulse, and blood glucose were inputted into the patient's mobile phone and the patient could view the measurements of blood pressure, pulse, and blood glucose, prescription and medication information, doctor appointments, and health information.
The physician had the patient's blood pressure, pulse, blood glucose, electrocardiogram, and X-ray images on the mobile phone for patient management.
The telecare service consists of Webdoc Plus to measure blood pressure, blood glucose and body fat, EP202 to measure the electrocardiogram, an electronic stethoscope capable of auscultating, storing and transmitting cardiac sounds, a webcam and a headset. The equipments are described in Table 1.
According to the survey asking 51 ambulatory patients from the cardiology and the thoracic and cardiovascular surgery clinics about their needs and intentions of using telemonitoring and telecare services, 37 patients (73%) responded affirmatively. They were willing to continue to use the service for the patients felt relieved that the doctor always observed them rather than that they had to visit the doctor's office in person. They also said that it will be even better if the medical staff perceives the patient's incognizable symptoms and guides them to medical treatment.
The telecare service basically consists of a PHD, a gateway, applications and server components. In this study, the system configuration comprises two kinds of devices and the electronic stethoscope as shown in Figure 1.
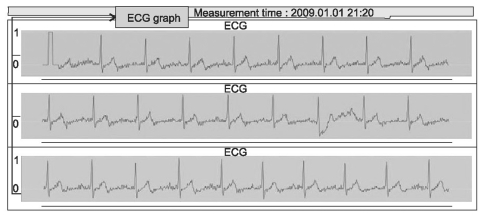
Figures 4-6 show the screen which you can view the measurement data of blood pressure, pulse, electrocardiograms, and body fat. The pulse and blood pressure appear on the graph to easily show the status. The subjects measured blood pressure, pulse and electrocardiogram 2-3 times a day and body fat 1 time a day on the average [10].
To receive video consultation services, the patient should click on the video consultation icon and type in the ID and password used to register when joining the service to log on.
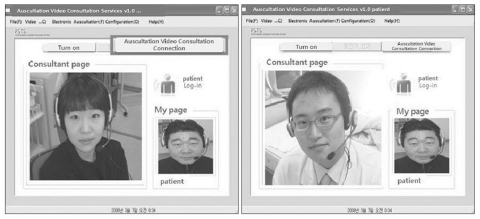
If the patient clicks the auscultation and video connection icon, the indication "connecting to monitoring personnel" appears and after a short time interval, the video consultation with monitoring personnel takes place (Figure 7).
The video consultation will be conducted while connected to monitoring personnel. When the patient needs a consultation with a physician, depending on the given circumstance, it is available instantly or after waiting for a certain time. If instant consultation is not available, the patient makes an appointment for a consultation and has a consultation at the reserved time.
When the patient consults a physician, if auscultation is necessary, the patient can use the on and off button of the electronic stethoscope (Figure 8).
Before commencement of the use of service, it is necessary to inform users of the terms of the use of service and receive a written consent to the service.
1) When patient information is typed in on the telecare website, the patient ID and password are generated.
2) The guidelines for the method of biometric data measurement and having experience in biometric data measurement help the aged patients use the devices by themselves by trying U-health measurement devices themselves at the experience hall of the U-healthcare center.
3) The user guidelines for the telecare website helps educate the service users who are not accustomed to using computers or have difficulty in using them, on the brief method of using computers and website at the experience hall of the U-healthcare center.
4) By experiencing the video consultation service and the electronic stethoscope test at the experience hall of the U-healthcare center, patients learn how to use the video consultation program and try actual video connection with a physician.
5) Visit the patient's home and install/loan the telecare measurement program and the device to measure biometric data compliant with the PC environment. After the installation, evaluate whether or not the service performs adequately.
6) By connecting the video consultation with a physician and testing the electronic stethoscope, conduct a video connection with a physician at home similar to the experience hall.
7) Continuously monitor the Result of Biometric Data Measurement. Periodic measurement of biometric data can be viewed on the webpage and the physician and monitoring personnel confirm the data on a daily basis. If any trouble arises, they provide necessary feedback.
8) With analyzing the periodically measured biometric data, the progress of the accumulated biometric data is clearly shown in a graph in the monthly 'newsletter.' During the visit to the patient's home, a variety of health information and exercise information is delivered and any inconvenience issues can be addressed.
The subjects of the pilot study were discharged after undergoing heart surgery from the Department of Thoracic Surgery. There were five females and five males: one in the twenties, three in the forties, four in the fifties, one in the sixties and one in the seventies. The subjects measured blood pressure, pulse and electrocardiograms 2-3 times, and body fat once a day. As a result of the survey on the level of satisfaction after the use of the service, the subjects all responded that it was necessary to measure blood pressure, pulse, blood glucose, and electrocardiograms regularly, and that using the device to measure physical information was effective for their health management. About whether to recommend the telecare service to others, > 90% responded that they would recommend the telecare service. If this telecare service becomes a paid service, it appeared that 50% of patients had an intention to pay 50,000 Korean won per month and 40% had an intention to pay 50,000-70,000 Korean won per month.
With the satisfaction level during the period of service, > 80% answered that they were satisfied. The strongest merit in this service was said to be "convenient healthcare" in 36%, and 36% answered "I feel relieved because somebody is always taking care of my health."
In addition, the major disadvantage of this service was that the equipment sometimes did not work properly or it was too big. They suggested the development of more practical devices, measurement to be done without switching on a PC and a convenient UI for the aged.
Based on the characteristics that heart disease patients are well-aware of everyday health care and do have a strong need for U-health services, a service of patient management after hospital discharge directly connected to a physician was established.
The subjects were mostly satisfied with the service and the use of devices and some subjects wanted to receive actual commercial services continuously apart from the period of the demonstration service. Although it was a comparatively short period, the subjects actively participated in this project and showed a high level of satisfaction.
According to the recent studies of Chaudhry et al. [11], the results of telemonitoring most of the cardiac failure patients appeared to be improved in the small studies and yet not to be proven in the large trial. This reference, however, is limited to collecting information on symptoms and responding by telephone, which shows some different service scope from our study. In the future, it is recommended that the system to enable teleconferencing services and data collection such as blood pressure, electrocardiograms and heart sounds at home be implemented targeting a large group of people for a certain period of time and the effect and satisfaction level be verified.
The telemedicine and telecare service should be applied to specific patients in special circumstances rather than general patients to achieve great effects and high level of satisfaction of physicians.
Therefore, because it was applied to cardiothoracic surgery specialists and heart surgery patients who have strong needs for physicians and patients, the satisfaction level with the service was high. For a certain period of time after heart surgery, telecare services seem suitable as a method of making it possible to carefully examine the patient's condition and reducing the patient's unnecessary visits to a medical institution as well as the inconvenience and the financial burdens by discerning anxiety and physical symptoms after surgery. The patients who need > 3-month services should be provided with personalized health information, such as diet and exercise, to leverage the effectiveness of constant management.
In addition, considering the issues and improvement regarding the measuring devices and a method of providing services during the pilot trial, in order for U-health services to be widely accepted in society and generalized, all of the measuring devices which collect biometric data and the service should be customized to the patient's disease and conditions. Accordingly, it is reckoned that the function which can be used with comparative ease and transmit the measured result without turning on a PC, and the UI which is more convenient to use are necessary. It will be also important to develop a model to provide the devices necessary for each disease in a package form and combine the contents and services into a customized service. To develop this kind of service, the development of general purpose healthcare devices and a service platform, a gateway for health data transmission, and the health data analysis engine should be preceded. If the continuous development of technology leads to generalizing the U-healthcare service and customized services for patients, it is expected that the service can be developed in a form in which physicians can prescribe U-health service suitable for the patient's condition, residential environment, family status and so on just like the traditional doctor's prescription, and then patients can accept and use it without any aversion or burden.
The limitations of this study are that the system target group was limited to one hospital and the significant age difference hindered varying the contents by age and IT friendliness.
It is recommended that the future study perform a large scale research and also develop the security system to protect personal information and age-specific contents to verify the satisfaction of the system and service.
Acknowledgements
This research was supported by Grant No. 10037283 from the Industrial Strategic Technology Development Program funded by the Ministry of Knowledge Economy.
This research was also supported by the Ministry of Knowledge Economy, Korea, under the Convergence-ITRC (Convergence Information Technology Research Center) support program (NIPA-2011-C6150-1101-0001) supervised by the National IT Industry Promotion Agency (NIPA).
References
1. Kang SW, Lee SH, Ko YS. The advent of u-health era. 2007. Seoul: Samsung Economic Research Institute.

2. Lee KH, Kim HJ. Fuzzy trust evaluation model for virtual telecare team. J Soc Korea Ind Syst Eng 2009;32:112-119.

3. Pare G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc 2007;14:269-277. PMID: 17329725.



4. Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334:942PMID: 17426062.



5. Delgado-Passler P, McCaffrey R. The influences of postdischarge management by nurse practitioners on hospital readmission for heart failure. J Am Acad Nurse Pract 2006;18:154-160. PMID: 16573728.


6. Brownsell S, Blackburn S, Hawley MS. Evaluating the impact of 2nd and 3rd generation telecare services in older people's housing. J Telemed Telecare 2008;14:8-12. PMID: 18318922.


7. Chaudhry SI, Phillips CO, Stewart SS, Riegel B, Mattera JA, Jerant AF, Krumholz HM. Telemonitoring for patients with chronic heart failure: a systematic review. J Card Fail 2007;13:56-62. PMID: 17339004.



8. Biddiss E, Brownsell S, Hawley MS. Predicting need for intervention in individuals with congestive heart failure using a home-based telecare system. J Telemed Telecare 2009;15:226-231. PMID: 19590027.


9. Carl M, Tracy F, James C, Catherine E, Claire G, K Neil J, Sur K, Frances M, Janice O, Louise R, Anne R, Rob W. Integrating telecare for chronic disease management in the community: what needs to be done?. 2010. Newcastle Upon Tyne, UK: Institute of Health and Society, Newcastle University.

10. Gil Telecare Service [Internet]. Gachon University Gill Medical Center. c1958-2008. cited at 2011 Jan 31. Incheon: Gachon University Gill Medical Center; Available from: http://gts.gilhospital.com/GTS

11. Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med 2010;363:2301-2309. PMID: 21080835.



-
METRICS

-
- 6 Crossref
- 3,305 View
- 39 Download
- Related articles in Healthc Inform Res