|
 |
- Search
| Healthc Inform Res > Volume 17(4); 2011 > Article |
Abstract
Objectives
The aim of this study was to develop and validate Detailed Clinical Models (DCMs) for nursing assessments and interventions.
Methods
First, we identified the nursing assessment and nursing intervention entities. Second, we identified the attributes and the attribute values in order to describe the entities in more detail. The data type and optionality of the attributes were then defined. Third, the entities, attributes and value sets in the DCMs were mapped to the International Classification for Nursing Practice Version 2 concepts. Finally, the DCMs were validated by domain experts and applied to case reports.
As health care grows more complex and the boundaries among health professionals become increasingly blurred, the ability to communicate effectively about patient care is more important than ever [1]. In addition, as health care organizations transition from paper to electronic documentation systems, data collected from an electronic documentation system should be able to be reused for a purpose other than the original; such as the continuity of care and decision support on the individual level, quality measurement, and management of healthcare institutions [2,3].
One of the main challenges of sharing and reusing healthcare data is the semantic interoperability of data collected. Semantic interoperability is defined as the ability for data shared by systems to be understood at the level of fully defined domain concepts [3,4]. Semantic interoperability ensures that exchanged information be understood by any other systems or applications not initially developed for [3,5].
To achieve semantic interoperability it is necessary to have standards, not just for terminology to represent data but also structure of data to be transferred [5]. One way to ensure semantic interoperability would be to represent data with standardized terminology, in which each clinical concept is unique and clearly defined. However, there is no terminology covering all domains of health care currently available. Besides a terminology to represent all concepts of health care is not realistic and thus not desirable [5-7]. In addition to standardized terminology to represent data collected, it is necessary to have data model to capture context where and how data were collected [7]. Data model expresses clinical concepts in a standardized and reusable manner [8]. One of data model called Detailed Clinical Models (DCMs) consists of entity-attribute-value triplets. An entity is a core or focus concept of a data element. An attribute is a qualifier that represents a data entity in more detail, and is associated with possible values. A value set, in turn, represents a uniquely identifiable set of valid concept representations of an attribute. These models represent the information a clinician may want or need to report about patients, which are highly related and clinically meaningful for clinicians. In addition, these models enable to create and systematically organize clinical information or knowledge in specific contexts to conform to requirements of data capture [7-11].
There have been several different researches to develop data models in health care. Examples are Intermountain Healthcare Clinical Element Models (CEMs), 13606/openEHR archetype, HL7 templates, Dutch Detailed Clinical Model, and Clinical Contents Model [12-15]. However, these efforts are limited to the domain of medical knowledge. Though the importance of developing data models in nursing has been addressed by many nurse informaticists [8], there is only one report on this topic in nursing literature by Goossen [16], except research results published by the authors of this paper [17-20]. Goossen [16] developed data specifications for stroke patients that have been developed in the Netherlands and the authors of this paper developed DCMs of nursing problems for breast cancer patients, nursing problems for maternal care, nursing assessment for cancer survivors, and nursing information for initial assessment in Korea. These researches were only pilot studies which showed the possibility of model development in nursing domain.
Therefore, it is necessary to develop data models to represent comprehensive nursing concepts covering patient health status and nursing activity. The purpose of the present study was to develop and validate DCMs to represent clinical contents of nursing assessments and interventions to be implemented in electronic nursing records.
This study was carried out in two steps: first, DCMs were developed by identifying entities, attributes, and values and linking them; second, DCMs were validated by the domain experts.
The entities, key concepts of data elements were extracted from various sources. First, we extracted entities by analyzing narrative nursing statements used to document nursing care in electronic nursing records system in a tertiary teaching hospital in Korea. For example, 'pain' entity was extracted from narrative nursing statements such as 'complain of pain', 'severe pain persist', 'acute pain in abdomen', 'RUQ pain present', and 'no pain in IV site'. Second, we extracted entities by reviewing concepts of International Classification for Nursing Practice (ICNP) version 2. Concepts such as 'hopelessness', 'colic pain', and 'drinking pattern' were extracted from ICNP version 2. Third, we extracted entities by reviewing nursing literatures and clinical practice guidelines. Concepts such as 'skin condition', 'back pain', and 'chemotherapy induced vomiting' were extracted from the nursing literatures and clinical practice guidelines.
The attributes of entities, which are qualifier or modifier to represent the entities in more detail, were also identified by analyzing narrative nursing statements; reviewing ICNP concepts, nursing literature, and clinical practice guidelines; and interviewing the domain experts. For example, we identified 'anatomical site' attribute from the following statements: 'pain in abdomen', 'pain in back', and 'RUQ pain'.
Then, we categorized attributes by referring to characterizing categories of the ISO/DTS 22789, a conceptual framework for patient findings and problems in terminologies [21], semantic domains of the ISO 18104, a reference terminology model for nursing [22], and qualifier values of the Systematized Nomenclature of Medicine Clinical Terms.
Possible values of attributes were identified again by analyzing narrative nursing statements; reviewing ICNP concepts, nursing literature, and clinical practice guidelines; and interviewing the domain experts.
We modeled DCMs by linking an entity and its corresponding attributes with values, and specifying data types and optionality of the attributes. Data type of attributes was selected from the ISO/DIS 20190 Health Data Type Standard [23]. Examples are 'BL: boolean', 'SC: character string with coded', 'INT: integer number', 'TS: point in time', 'CO: coded ordinal', 'REAL: real number', and 'ST: character string'. Optionality of attributes was specified by interviewing domain experts. Optionality of attributes can be either mandatory (attribute must be used) or optional (attribute may be used).
Then, we conducted an internal validation. During internal validation, each model was refined through reviewing the similar entities, related entities, and opposite entities and through repeated consultation with domain experts. The concepts in entity-attribute-value triplets of DCMs were mapped to ICNP version 2, which is a reference terminology in nursing.
The adequacy of DCMs was validated by eight domain experts who were nurses with graduate level informatics training and clinical nursing experience more than five years. To ensure reliability of validation among eight experts, the experts were taught validation process with 10 DCMs. The experts then validated additional 40 DCMs randomly assigned to them using questionnaire for inter-rater reliability. In the questionnaire, experts were asked whether the entities were clearly represented and reusable in nursing practice; attributes and value sets were mutually exclusive, inclusive, consistent, and relevant to represent entities; and data type and optionality of each attribute were relevant to represent entities. The items of the questionnaire were scored on 4-point rating scale (from 1 = strongly disagreed to 4 = strongly agreed). We asked the experts to provide comments when they rated DCMs with score 1 or 2. Inter-rater reliability was 0.782 (p = 0.016).
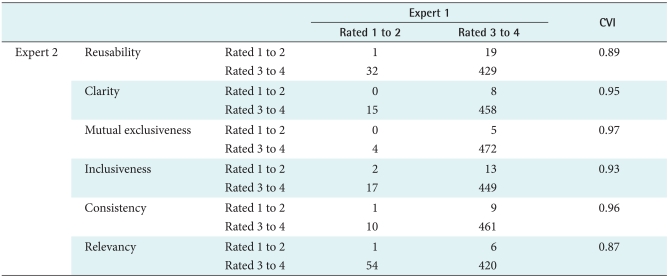
For actual validation, four groups of two experts validated 481 DCMs. We calculated a content validity index (CVI) for the validation of the DCMs. A CVI of 0.80 or higher is generally acceptable [24,25].
After validation, we invited all of the eight domain experts and convened a meeting to further discuss DCMs with score 1 or 2. In the meeting, each expert explained why they rated specific DCMs with score 1 or 2. These DCMs were refined by the consensus building process among eight experts.
In total, 429 entities of nursing assessments and 52 entities of nursing interventions were extracted. Three hundred seventy five entities (77.9%) were extracted from narrative nursing statements, 61 entities (12.7%) from ICNP version 2, and 45 entities (9.4%) from nursing literatures and clinical practice guidelines.
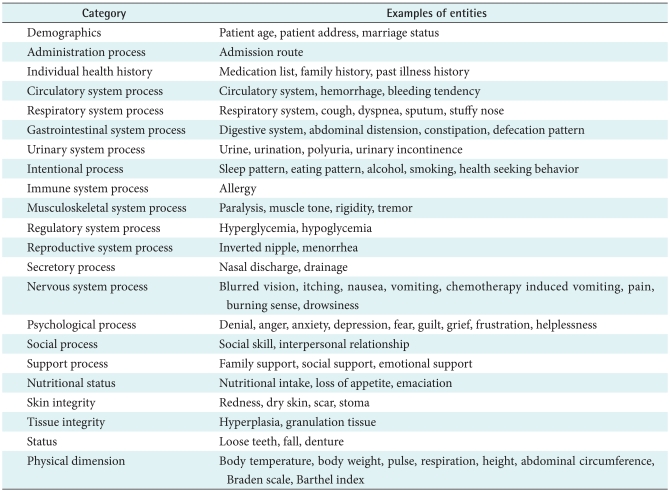
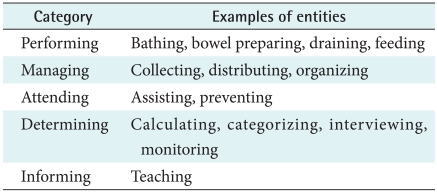
Entities of nursing assessments were classified into 22 categories such as demographics, administration process, and intentional process (Table 1). Entities of nursing interventions were classified into five categories such as performing, managing, attending, determining, and informing (Table 2). Attributes concepts of nursing assessments were classified into 11 categories such as timing, anatomical site, target, and degree (Table 3). Attributes concepts of nursing interventions were classified into 11 categories such as target, means, and recipient (Table 3).
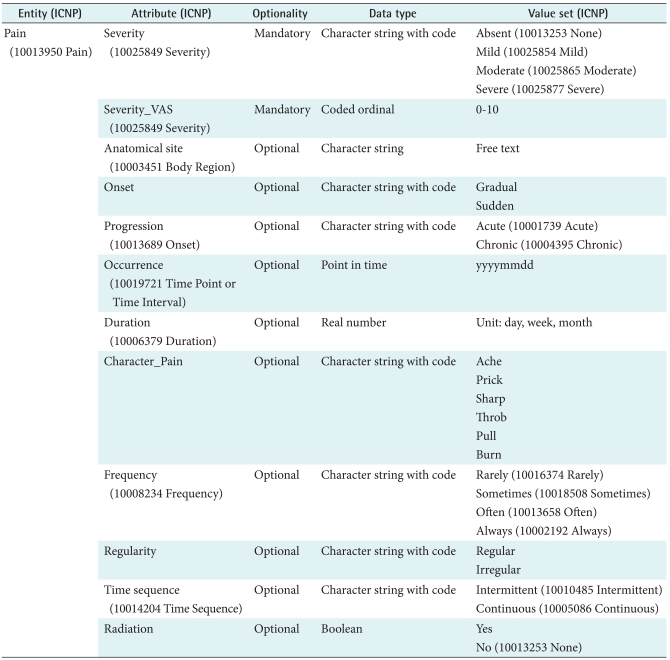
Table 4 depicts 'pain' DCM as an example DCM of nursing assessments. 'Pain' DCM has 12 attributes, including severity, severity_VisualAnalogueScale, anatomical site, onset, progression, occurrence, duration, character_pain, frequency, regularity, time sequence, and radiation. Four concepts were identified as values to express severity of pain and were mapped to ICNP concepts. Data type of severity attribute was expressed in a coded value. To describe pain, severity attribute was necessary, and other attributes were desirable. Entities, attributes, and values concepts were mapped to ICNP version 2 concepts. For example, 'pain' was mapped to '10013950 Pain' of ICNP.
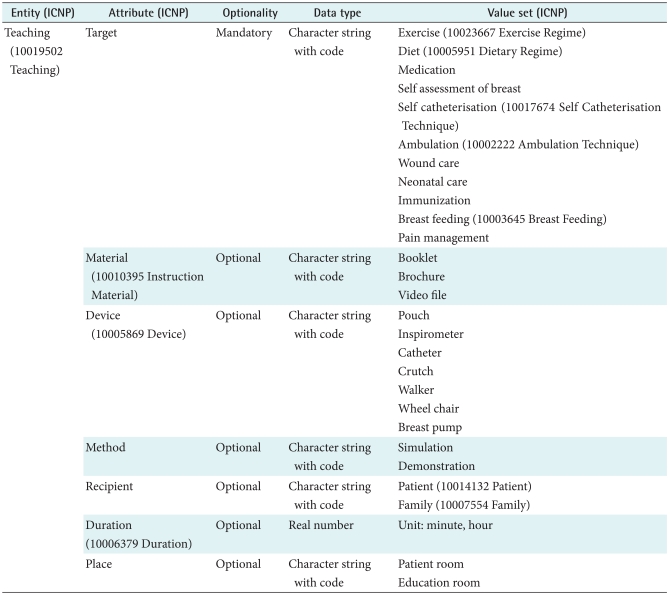
'Teaching' DCM as example DCM of nursing interventions was presented in Table 5. 'Teaching' entity has seven attributes: target, material, device, method, recipient, duration, and place. Concepts such as exercise, diet, wound care, and ambulation were identified as values of target attribute of teaching DCM. Data type of target attribute was a coded value. To describe teaching, target attribute is required and material, device, method, recipient, duration, and place attributes are recommended. Entities, attributes, and values concepts were mapped to ICNP version 2 concepts. For example, 'teaching' was mapped to '10019502 Teaching' of ICNP.
CVI between the two experts ranged from 0.87 to 0.96 (Table 6). A CVI score of 0.80 or better is generally considered to have a good content validity. DCMs rated as either 1 or 2, in total 115 DCMs, were modified and refined. The domain experts rated 4 DCMs as either 1 or 2 for irrelevant naming of entities. They suggested changing names of the entities to clearly reflect nursing practice. 'Vascular pain' was renamed to 'phlebitis' based on the suggestion of nurse experts.
They rated 12 DCMs as either 1 or 2 for incompleteness of attributes and values. They suggested adding additional attributes and values. For example, 'alcohol' DCM originally has four attributes, including previous alcohol consumption, current alcohol consumption, amount, and duration of alcohol consumption. Frequency of alcohol consumption attribute was added to the 'alcohol' model. They rated 54 DCMs as either 1 or 2 for inconsistency of attributes and values. They suggested adding attributes and values to describe the presence or absence of each entity in DCMs. If it is important to document absence of a problem, such as pain and discomfort, we added presence/absence attribute with absent as one of value set. On the other hand, if it is not important to document absence of a problem, such as macular, we did not add presence/absence attribute.
They rated 45 DCMs as either 1 or 2 for irrelevant optionality of attributes. For example, optionality of severity attribute of 'depression' DCM was changed from optional to mandatory based on the recommendation of the experts.
The purpose of this study was to develop DCMs for nursing assessments and interventions. We developed 481 DCMs in this study, which is about 1.5 times more than the number of archetypes developed in the openEHR for the entire domain of medicine [26]. The DCMs we developed had covered content of patient problems and nursing activity.
When we identified attributes of the entities, we found small number of attributes from narrative nursing statement such as severity, presence or absence, and increase or decrease of signs and symptoms. This implies that nurses do not document nursing assessment as precisely as described in the literature or as recommended by the domain experts [18].
We also encountered a few challenges during the development of DCMs. The first challenge was how to select nursing sensitive entities for DCMs in nursing. Entities we identified could be classified as entities for nursing only problems such as self esteem and disturbed body image; entities for shared problems between nursing and medicine such as unconsciousness, pain, and malnutrition; and entities for medicine only problems such as spider hemangiomas. We decided not to develop DCMs for entities for medical problems in this study. The DCMs we developed for shared problems between nursing and medicine could have different attributes from DCMs developed in medicine, because nurses view and document the same entity differently from other health care professionals. For example, blood pressure can be represented with various attributes such as anatomical site, position, cuff size, and device. However, 'blood pressure' DCM we developed does not have attributes such as confounding factor found in the 'blood pressure' model developed in medicine because it is not easy for nurses to make judgment on contributing factors to the blood pressure [26]. Data can be shared between nursing and medicine domains as long as the structure and meaning of data are the same. However, if structure and meaning of data are not the same, complex interfaces are required to share data between nursing and medicine domains.
The second challenge we faced was that entities have different abstract levels. For example, musculoskeletal pain is a super concept of arthritis pain, bone pain, and muscle pain. Another example is the relationship between pain and labor pain which is a type of pain. One way to reflect different abstract level in DCMs would be to introduce the hierarchies of DCMs.
The third challenge we faced was that entities can be nested. To avoid nesting problem in nursing assessment DCMs, we did not include related or contributing factors to patient problems in DCMs. For example, 'coughing' DCM could have 'allergy' as one of related factors, which can be modeled separately. We removed nesting problem in nursing intervention DCMs by excluding qualifying or modifying factors. For example, 'assessing' DCM could have 'discharge' as one of assessment target with its own attributes and value sets, which can be modeled as a separate patient problem.
We found that value set of attributes developed for a DCM can be reused in the other DCM. For example, value set of severity attribute describing degree of pain in 'pain' DCM can be reused in describing degree of febrile sense. We also found that two different DCMs can have exactly the same attributes and value sets. For example, 'grief' and 'guilt' DCMs have the same attributes such as severity, progression, duration, frequency, onset, and occurrence with the same value sets. These findings imply reusability of the attributes and value sets in DCM development.
The DCMs developed in this study were validated by the domain experts. The domain experts rated reusability, clarity, mutual exclusiveness, inclusiveness, consistency, and relevancy of the DCMs on a 4-point scale (from 1 = strongly disagreed to 4 = strongly agreed). This validation method was used because there are no tools and gold standards available to evaluate the quality of the data models such as DCMs. Quality and usability of the DCMs developed in this study can be further evaluated when these models are implemented in the electronic nursing records system.
DCMs of nursing assessments and interventions were developed to represent comprehensive contextual data and information in a more consistent manner. The DCMs developed in this study can be used in the electronic nursing record system to ensure semantic interoperability of nursing data. DCMs can be used for both structured and unstructured data entry in the electronic nursing records system. For structured data entry, DCMs can be used for designing sections and templates of nursing forms. For unstructured data entry, DCMs can be used to generate narrative statements. Once the DCM-based electronic nursing record system is developed, it is expected to see the improvement in the quality of data collected in terms of reusability, portability, granularity, flexibility, and redundancy, and quality of nursing care in terms of patient outcomes.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (No. 2009-0074695) & (No. 2011-0018261).
References
1. Urquhart C, Currell R, Grant MJ, Hardiker NR. Nursing record systems: effects on nursing practice and healthcare outcomes. Cochrane Database Syst Rev 2009;(1):CD002099PMID: 19160206.


2. Goossen W, Goossen-Baremans A, van der Zel M. Detailed clinical models: a review. Healthc Inform Res 2010;16:201-214. PMID: 21818440.



3. Garde S, Knaup P, Hovenga E, Heard S. Towards semantic interoperability for electronic health records. Methods Inf Med 2007;46:332-343. PMID: 17492120.


4. Elkin PL, Froehling D, Bauer BA, Wahner-Roedler D, Rosenbloom ST, Bailey K, Brown SH. Aequus communis sententia: defining levels of interoperability. Stud Health Technol Inform 2007;129(Pt 1):725-729. PMID: 17911812.


5. Stroetmann V, Jung B, Rector A, Rodrigues J, Ustun B, Lewalle P, Dobrev A, Kalra D. Semantic interoperability deployment and research roadmap. 2007. Brussel, Belgium: The European Commission.

6. Park HA, Hardiker N. Clinical terminologies: a solution for semantic interoperability. J Korean Soc Med Inform 2009;15:1-11.

7. Beale T. Archetypes: constraint-based domain models for future-proof information systems. Workshop on Behavioural Semantics (Object Oriented Programming Systems Languages 2002); 2002 Nov 4-8. Washington, USA.

8. International Organization for Standardization (ISO). Health Informatics: quality criteria and methodology for detailed clinical models. International Organization for Standardization. ISO/CEN/Working Draft 13972. 2009. Geneva, Switzerland: ISO.

9. Hovenga E, Garde S, Heard S. Nursing constraint models for electronic health records: a vision for domain knowledge governance. Int J Med Inform 2005;74:886-898. PMID: 16115795.


10. Garde S, Hovenga E, Buck J, Knaup P. Expressing clinical data sets with openEHR archetypes: a solid basis for ubiquitous computing. Int J Med Inform 2007;76(Suppl 3):S334-S341. PMID: 17392019.


11. Coyle JF, Mori AR, Huff SM. Standards for detailed clinical models as the basis for medical data exchange and decision support. Int J Med Inform 2003;69:157-174. PMID: 12810120.


12. Huff SM, Rocha RA, Coyle JF, Narus SP. Integrating detailed clinical models into application development tools. Stud Health Technol Inform 2004;107(Pt 2):1058-1062. PMID: 15360974.


13. International Organization for Standardization (ISO). Health informatics: electronic health record communication - Part 3: Reference archetypes and term lists. ISO 13606-2. 2008. Geneva, Switzerland: ISO.

14. Goossen WT. Using detailed clinical models to bridge the gap between clinicians and HIT. Stud Health Technol Inform 2008;141:3-10. PMID: 18953119.


15. Ahn SJ, Kim Y, Yun JH, Ryu SH, Cho KH, Kim SW, Kim SS, Kwak MS, Yu SJ, Koh YT, Choi DJ. Clinical contents model to ensure semantic interoperability of clinical information clinical contents model to ensure semantic interoperability of clinical information. J KIISE Softw Appl 2010;12:871-881.

16. Goossen WT. Intelligent semantic interoperability: integrating knowledge, terminology and information models to support stroke care. Stud Health Technol Inform 2006;122:435-439. PMID: 17102295.


17. Min YH, Park HA. Development and validation of archetypes for nursing problems in breast cancer patients. J Korean Soc Med Inform 2009;15:393-401.

18. Kim Y, Park HA. Development and validation of detailed clinical models for nursing problems in perinatal care. Appl Clin Inform 2011;2:225-239.



19. Lee MK, Park HA. Development of data models for nursing assessment of cancer survivors using concept analysis. Healthc Inform Res 2011;17:38-50. PMID: 21818456.



20. Kim YR, Park HA, Min YH, Lee MK, Lee YJ. Development of detatiled clinical models of nursing information for initial assessment. J Korean Clin Nurs Res 2011;17:101-112.

21. International Organization for Standardization (ISO). Conceptual framework for patient findings and problems in terminologies. ISO/TC215: 22789. 2010. Geneva, Switzerland: ISO.

22. International Organization for Standardization (ISO). Health informatics: integration of a reference terminology model for nursing. ISO/TC215: 18104. 2003. Geneva, Switzerland: ISO.

23. International Organization for Standardization (ISO). Health informatics: harmonized data types for information interchange. ISO/TC215: 21090. 2011. Geneva, Switzerland: ISO.

24. Kim HY, Cho IS, Lee JH, Kim JH, Kim Y. Concept representation of decision logic for hypertension management using SNOMED CT. J Korean Soc Med Inform 2008;14:395-403.

25. Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health 2006;29:489-497. PMID: 16977646.


26. Clinical knowledge manager [Internet]. OpenEHR Foundation. 2007. cited at 2010 Aug 20. London, UK: OpenEHR Foundation; Available from: http://www.openehr.org/knowledge/

-
METRICS

-
- 4 Crossref
- 3,945 View
- 36 Download
- Related articles in Healthc Inform Res
-
Development of a Standardized Curriculum for Nursing Informatics in Korea2022 October;28(4)