Review of Qualitative Research Methods in Health Information System Studies
Article information
Abstract
Objectives
The aim of this study was to review hospital-based health information system (HIS) studies that used qualitative research methods and evaluate their methodological contexts and implications. In addition, we propose practical guidelines for HIS researchers who plan to use qualitative research methods.
Methods
We collected papers published from 2012 to 2022 by searching the PubMed and CINAHL databases. As search keywords, we used specific system terms related to HISs, such as “electronic medical records” and “clinical decision support systems,” linked with their operational terms, such as “implementation” and “adaptation,” and qualitative methodological terms such as “observation” and “in-depth interview.” We finally selected 74 studies that met this review’s inclusion criteria and conducted an analytical review of the selected studies.
Results
We analyzed the selected articles according to the following four points: the general characteristics of the selected articles; research design; participant sampling, identification, and recruitment; and data collection, processing, and analysis. This review found methodologically problematic issues regarding researchers’ reflections, participant sampling methods and research accessibility, and data management.
Conclusions
Reports on the qualitative research process should include descriptions of researchers’ reflections and ethical considerations, which are meaningful for strengthening the rigor and credibility of qualitative research. Based on these discussions, we suggest guidance for conducting ethical, feasible, and reliable qualitative research on HISs in hospital settings.
I. Introduction
Health information systems (HISs) are designed to improve patient health and safety in healthcare settings. These systems support the administrative and management tasks necessary for medical and nursing services, using standardized clinical patient data. These data are utilized for patient treatment, healthcare plans, and clinical research, thereby improving the healthcare environment [1]. Additionally, the effective use of HISs contributes to improving hospital management efficiency and helps achieve cost savings [2,3]. Therefore, HISs play an essential role in current healthcare services.
Over the last few decades, medical settings have widely adopted information technologies. However, despite the progress made in HISs, several issues have emerged concerning the optimization and utilization of HISs in hospitals [4]. These problems and challenges arise at various levels. For instance, there are macro-level issues related to the external environment and policies, conflicting perspectives among stakeholders, changes in work practices, unintended consequences within hospital organizations, and resistance among users. Therefore, it is crucial to consider personal, social, psychological, and physical aspects beyond the system engineering and design approach to understand and address the limitations associated with HISs.
Recent HIS studies have taken a multidisciplinary approach, incorporating theories and methods from various fields such as sociology, anthropology, organizational studies, and systems engineering. These studies aim to identify problems and provide recommendations for improving HISs [5–10]. For example, the Systems Engineering Initiative for Patient Safety is a framework focusing on the interaction between human and computer system elements to support work performance and patient safety when HISs are used [5]. Other frameworks have proposed process-oriented research methods and perspectives to identify the unintended consequences of HIS applications. These studies consider the actors who use the system and utilize a socio-technical perspective to recognize problems and propose solutions [6–8]. They consider multiple dimensions of the individual, organization, system, and environment to provide a holistic approach to addressing HIS-related issues.
In HIS studies, qualitative research methods offer a perspective that helps to understand and interpret phenomena, meanings, and context. Some HIS researchers emphasize qualitative methodologies to capture personal and social factors surrounding systems [10] and understand the contextual meaning, including social, cultural, organizational, and political issues related to information technology [11]. Moreover, qualitative methods are useful for uncovering psychological and sociocultural factors that are difficult to capture with quantitative research methods. In other words, qualitative research can contribute to person-centered healthcare by examining multilayered and complex contexts among actors surrounding information systems.
However, there are still many challenges in applying qualitative research methods in studies on information systems in general. For example, one common criticism is that qualitative studies may lack objectivity, making it difficult to generalize the results and ensure methodological rigor. The perspectives and interpretations of researchers often influence the outcomes, necessitating systematic approaches to maintain research rigor [9,12,13]. Moreover, qualitative researchers must interact with study participants, which requires attention to ethical dilemmas as they arise at the moment [14]. Therefore, assessing the reflexivity of qualitative researchers and the ethical considerations they employ during the research process is crucial for strengthening the rigor and credibility of qualitative research.
Therefore, this study aimed to conduct a review of researcher characteristics and reflections, research participant sampling, and data collection and management processes reported in participatory observations, in-depth interviews, and focus group interviews (FGIs) used in existing hospital-based HIS research. It is hoped that this article will provide contextual considerations and insights to help researchers conduct ethical, feasible, and reliable qualitative HIS research in hospital settings.
II. Methods
1. Research Questions
This study set out to address the following research questions dealing with qualitative research methods within the field of HISs:
What research processes are reported in participant observation, in-depth interviews, and FGIs of hospital-based HISs and related people with respect to researcher characteristics and reflection, participant sampling, and data collection and analysis?
What are the ethical and practical dilemmas in qualitative research found in the reported research process?
2. Search Strategy
We searched for qualitative research methods in HIS studies to collect articles published from 2012 to 2022 using the PubMed (MEDLINE) and CINAHL databases, referring to the COSI model, a literature search protocol for health technology assessment proposed by the U.S. National Library of Medicine [15].
The search terms were strategically made by combining three categories: types of HISs, operational terms such as “implementation” or “adaptation,” and qualitative research methods. It is useful to enter these multiple search terms because it allows for a more targeted search that matches the research objectives. It has also been demonstrated to be highly reliable, comparable to manually searching articles using a single search term [16]. Table 1 shows the search commands for merging several terms.
3. Study Selection
We found 4,607 articles in PubMed (MEDLINE) and 553 articles in CINAHL following the search strategy and identified 4,872 articles after excluding 288 duplications. After identifying the research articles, two researchers decided on inclusion/exclusion criteria in a meeting. We limited the language of our search to English. We excluded pilot research, clinical reports, policy study reports, any studies not published in peer-reviewed journals, only study abstracts published, or where the full text was unavailable. The inclusion criteria were: (1) the study is relevant to the HIS technology included in the search keywords; (2) the study reports appropriate empirical data and findings on implementing and adapting an HIS in a hospital setting; (3) the research participants must be involved in the hospital and HIS development industry; and (4) the study utilizes representative qualitative research methods (i.e., participant observation, in-depth interviews, and FGIs).
Two researchers independently reviewed the article titles and abstracts based on inclusion/exclusion criteria. After reaching a consensus, 284 articles were selected. The researchers then reviewed the full text of these articles and excluded irrelevant studies in a subsequent meeting. After this review, 74 articles were selected that matched the objective of the study, which is to investigate qualitative research methods applied in the HIS field. Figure 1 shows the process of study selection.
4. Data Analysis
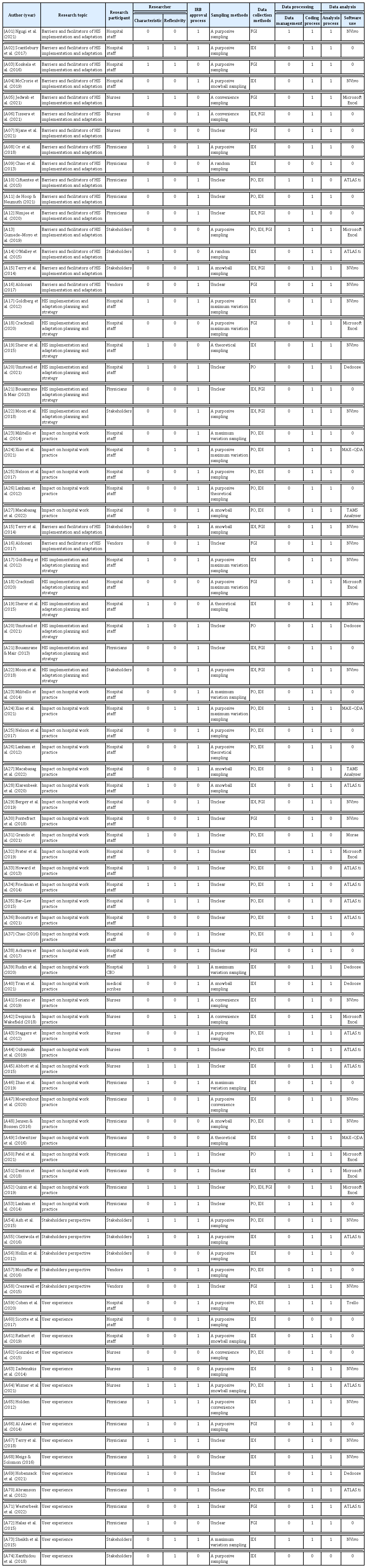
Two authors used the Standards for Reporting Qualitative Research (SRQR) checklist to analyze the research process of selected articles [17]. According to the SRQR developers, the checklist is a list of key factors that should be reported in utilizing qualitative research methods rather than criteria to be used to evaluate qualitative research. Therefore, we used it to determine which data to extract from the papers. To ensure the rigor of this research, we repeatedly validated the analysis while forming categories based on extracted data. We used Zotero as a bibliography management program and Microsoft Excel to organize the selected papers. A summary of the selected articles is shown in Table 2 and Appendix 1.
III. Results
Applying the SRQR checklist, we found that many of selected articles did not report their research methods in a detailed and systematic manner (Tables 3–6). About a quarter of the studies had no information on the ethical approval process. In some studies, limited reporting prevented a clear description of how research participants were identified or recruited. In general, selected studies did not include researcher characteristics, reflexivity, or data privacy during data collection.
1. Researcher Characteristics and Reflexivity
The characteristics of the researchers and interviewers were briefly reported in terms of qualitative research experiences or professional roles, such as doctoral students, nurse practitioners, or clinicians. A few studies reported collaborative work with medical specialists. Some articles indicated they had received additional training in qualitative research methods or HIS utilization to conduct research in hospital settings [A14, A17, A19, A28, A47, A66]. In the context of multi-disciplinary research teams engaging in HIS research, some articles reported a variety of researchers’ backgrounds, including health informatics, clinicians, nurses, and social scientists [A10, A52, A54, A70].
It was rare for authors to provide information about the researchers’ position, role, and impact on the study participants or settings. Only a few studies mentioned having no prior relationship with the research participants [A20]. Moreover, researchers rarely described the observer’s role and interactions with the participants in participant observation studies. However, they sometimes briefly reported how they intended to avoid influencing the participants during data collection and analysis. For example, researchers asked participants to confirm the collected data during interviews and observations, described procedures to minimize potential bias in data processing and analysis [A02, A05, A34, A50, A53, A54], or scheduled data collection at the participants’ convenience to avoid disrupting hospital workflows [A35].
2. Participant Sampling, Identification, and Recruitment
The findings related to participant sampling, identification, and recruitment are presented in Table 5. These findings were determined by reviewing the research methods. The most common sampling method was purposive sampling, in which researchers primarily used hospital expert databases or previous research records to identify participants with specific knowledge or experience in HIS utilization or selected participants with changing characteristics and information-rich cases. At the purposefully selected study sites, some researchers utilized convenience sampling to expand the diversity of sample characteristics [A47, A65], maximum variation sampling until new information emerged [A17, A18, A24], or snowball sampling, in which participants were referred to other potential participants during observations or interviews [A04, A61, A65].
Most studies provided detailed information about the study setting, but only a few described the process of selecting the sites and the contact made with them. In cases where the identification of participants was reported, researchers identified potential participants during site visits, which was mostly done through participatory observation. Researchers visited sites as part of a preliminary survey and attended hospital meetings or workshops.
Participants in studies were recruited through various methods, such as personal invitations, emails, and telephone contacts made by researchers. Researchers used emails, flyers, and posters to encourage interested individuals to get in touch voluntarily to express their interest in participating in the study. Although researchers identified potential participants through field contact, we noticed that some studies recruited participants through direct invitations by the researchers or bulk mail sending. This was mainly because the researchers also worked as clinicians or nurses and thus fulfilled dual roles.
3. Data Collection, Processing, and Analysis
Table 6 presents a comprehensive review of data collection, processing, and analysis. The data were collected using one or more methods, including participatory observation, in-depth interviews, and FGIs. According to the data presented in Table 6, in-depth interviews were conducted in 29 instances, participatory observation with in-depth interviews was done in 23 studies, and FGIs were utilized in 12 studies.
Among the studies that specified the data collection process, studies that utilized participatory observation specified and pseudonymized the study site, describing the bed size, hospital staff, and brief information about the implementation and adaptation process of HISs. Studies that reported the use of participatory observation generally described the scope and interaction of observation, with some stating that they used shadowing to avoid disruption or to collect more accurate observations [A23, A31, A34, A50, A52, A64, A70].
In the studies that reported interview locations, the designated places varied, including private clinic rooms, conference rooms, and break rooms. However, the interview location was often unspecified or not stated as a private room for security or confidentiality. This suggests that data were collected by conducting informal interviews during observation or by using interview transcripts and field observation notes to answer questions as they arose.
Some studies reported conducting interviews over the phone or virtual meetings when recruiting participants for large-scale studies or due to concerns about the coronavirus disease 2019 pandemic [A01, A17, A28, A39, A67, A71]. Some studies intentionally conducted interviews during lunch or other breaks to minimize disruption [A66].
The authors of the selected papers ensured that participants’ identities were anonymized during data collection and analysis. Some authors specified how data were stored [A23, A48, A60, A64, A68, A72], but most studies did not. Only a few authors requested feedback and revisions of the manuscript from their participants [A20], considering their impact on participants. Certain studies stipluated in their ethical approval procedure that the dataset should be shared only within the research team [A40, A41, A59].
Researchers frequently utilized qualitative research software during data processing and analysis. NVivo was used in 19 of the selected papers, ATLAS.ti in 14, and Microsoft Excel in 8. There were 24 articles that did not state which software, if any, was used. All papers generally described the coding and analysis process. The most commonly reported technique to enhance trustworthiness was member checking among researchers. However, no study specified participant involvement in the review.
IV. Discussion
Researchers must provide detailed information about their characteristics, sampling, and data collection and analysis when conducting qualitative research in hospital-based HISs. This is essential for strengthening the rigor and credibility of research [18]. However, the selected articles we reviewed did not meet these requirements for providing adequate detail. As a result, the credibility of qualitative research results may be compromised.
To establish credibility in hospital-based research, examining how the research process influenced the findings is essential. Ethical considerations related to accessing hospital sites, recruiting participants, and providing detailed information about the data collection and analysis process are critical. However, providing a principled recommendation about researchers’ access to and sampling of hospitals may not be feasible because hospital-based research is specific to each specialty.
Nevertheless, a detailed examination of procedures regarding the process of sampling, data collection, and the analysis of study participants will help researchers consider whether they can apply the methods used by other researchers to their situations. In summary, it is essential for researchers to consider ethical considerations regarding the research process to strengthen the credibility of qualitative research results. We discuss some key points highlighted in the review below.
1. Qualitative Research Rigor and Ethical Dilemmas
The rigor of qualitative research is strengthened by an explicit description of the researcher’s position and role in relation to the subjects of the study [14]. Researchers must continue to consider this requirement beyond the formal ethical approval process. However, around half of the selected articles did not provide details about the researcher or interviewer. Moreover, many clinicians or nurse researchers tended to use their workplace as the research site to conduct qualitative research in hospital settings. While this has obvious advantages for the research site, it is important to consider whether one is a researcher or a hospital worker throughout the research process. For example, if researchers are clinicians or nurses, can they remain neutral from an outsider’s perspective when investigating personal and social factors in HIS utilization? In a place that is both a workplace and a research site, can the researcher address concerns about patient care and privacy?
This also implies ethical and practical dilemmas regarding participant observation and research data collection in hospital-based research [18,19]. Formal ethical approval procedures require researchers to provide informed consent and notice to participants of their participation in the study. However, there is a practical challenge in obtaining informed consent in participatory observational research [20]. This challenge is further amplified when the research is conducted in a hospital setting, which is complex and unpredictable. For instance, in a large and busy environment like the emergency department, obtaining consent from everyone who may come under the scope of observation is extremely difficult. Furthermore, it is difficult in practice to fully explain the scope of the observation area to participants and to limit the data they collect to the scope of observations. The dilemmas associated with conducting qualitative research in the HIS field are considerable, as more than a third of the selected articles adopted participant observation as their primary research method. As a result, it is important for researchers to continually reflect on their position, role, and data collection at the beginning of a project and not just rely on considerations of the ethical approval process [19].
2. Sampling and Accessibility
When researchers access medical settings for their studies, they must deal with multiple stakeholders, not just formal ethical approval. The articles that reported participant sampling generally used a purposive sampling technique, in which researchers selected or invited participants, in that the nature of HIS studies is to target participants and settings with specific expertise [12,22]. It is, therefore, important to discuss whether they have selected appropriate sampling methods. This convenience and accessibility coinciding with the purpose of the study runs up against an inevitable issue—namely, the potential for biased selection by the researcher in the process of identifying and recruiting research participants. This dilemma needs to be fully discussed in hospital-based qualitative research [22].
As we reviewed the researcher’s position and role, we noted that many clinicians and nurses decided to conduct research within their workplace. This approach allows researchers to have a dual role in a hospital setting, making it easier to identify and recruit participants. If the study aims to improve the implementation or adaptation of HISs, including examples of successes and failures may be useful. However, researchers must be clear that selecting a research setting based on accessibility is intentional [19]. It is essential to recognize that the researcher’s perceptions and decisions about accessibility can affect the research design and process of carrying out the research [23,24].
3. Data Management and Privacy
Privacy can be compromised in healthcare settings during participant recruitment and data collection. The increasing use of HIS has expanded access to personal health records and, subsequently, the number of stakeholders collecting, using, and sharing them. This has raised new ethical, privacy, and trust issues [25,26]. While discussions on patient privacy are ongoing [18,27], privacy concerns for healthcare professionals who become research participants are often overlooked. Several researchers stated that they had gone through ethical procedures regarding the privacy and confidentiality of the research participants, but most of the selected articles did not provide details on how the data from participants were managed. This may be due to researchers’ potential bias toward participants whose records exist on websites and official healthcare databases. Therefore, researchers conducting HIS research in hospital settings need to consider the confidentiality and privacy of the research participants, who are often represented as experts in specific knowledge.
In participant observation studies, researchers observe healthcare work practices related to HIS utilization. As part of this process, the researcher may observe the computer screen, which can pose a significant risk of privacy violations when recording observational data. Due to the system features of HISs, direct personal information of medical workers and patients would be coded, but the researcher could inadvertently capture medical records and notes. As discussed earlier, this is a realistic limitation of participatory observation, but it is crucial to consider the presence of such information when categorizing and writing field notes [12,19].
In conclusion, although qualitative research has been used to study hospital-based HISs and the people who use them, there needs to be more examination of researcher characteristics and reflections, participant sampling, and data collection and management in the hospital setting. Given these issues, it is essential to assess the qualitative research methods utilized in hospital-based HIS research and discuss ethical and practical considerations and issues that require researchers’ attention.
4. Limitations
Two databases were used in this study to obtain numerous samples based on our search criteria. However, it is important to note that most of the studies included in the review were from the United States and Europe, which may require different approaches to hospital settings and HISs. While we reviewed and reported on qualitative research methods in general, other factors related to research data analysis were not examined in detail.
Acknowledgments
This work was supported by the research fund of Hanyang University (No. HY-202100000000317) and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MIST) (No. 2021R1G1A1092903).
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
Appendix
Appendix 1 Selected articles
A01. Ngugi PN, Were MC, Babic A. Users’ perception on factors contributing to electronic medical records systems use: a focus group discussion study in healthcare facilities setting in Kenya. BMC Med Inform Decis Mak 2021;21(1):362. https://doi.org/10.1186/s12911-021-01737-x
A02. Scantlebury A, Sheard L, Watt I, Cairns P, Wright J, Adamson J. Exploring the implementation of an electronic record into a maternity unit: a qualitative study using Normalisation Process Theory. BMC Med Inform Decis Mak 2017;17(1):4. https://doi.org/10.1186/s12911-016-0406-0
A03. Koskela T, Sandstrom S, Makinen J, Liira H. User perspectives on an electronic decision-support tool performing comprehensive medication reviews: a focus group study with physicians and nurses. BMC Med Inform Decis Mak 2016;16:6. https://doi.org/10.1186/s12911-016-0245-z
A04. McCrorie C, Benn J, Johnson OA, Scantlebury A. Staff expectations for the implementation of an electronic health record system: a qualitative study using normalisation process theory. BMC Med Inform Decis Mak 2019;19(1):222. https://doi.org/10.1186/s12911-019-0952-3
A05. Jedwab RM, Manias E, Hutchinson AM, Dobroff N, Redley B. Understanding nurses’ perceptions of barriers and enablers to use of a new electronic medical record system in Australia: a qualitative study. Int J Med Inform 2021;158:104654. https://doi.org/10.1016/j.ijmedinf.2021.104654
A06. Tissera S, Jedwab R, Calvo R, Dobroff N, Glozier N, Hutchinson A, et al. Older nurses’ perceptions of an electronic medical record implementation. Stud Health Technol Inform 2021;284:516-21. https://doi.org/10.3233/SHTI210786
A07. Njane A, Jedwab R, Calvo R, Dobroff N, Glozier N, Hutchinson A, et al. Perioperative nurses’ perceptions pre-implementation of an electronic medical record system. Stud Health Technol Inform 2021;284:522-7. https://doi.org/10.3233/ SHTI210787
A08. Or C, Tong E, Tan J, Chan S. Exploring factors affecting voluntary adoption of electronic medical records among physicians and clinical assistants of small or solo private general practice clinics. J Med Syst 2018;42(7):121. https://doi. org/10.1007/s10916-018-0971-0
A09. Chao WC, Hu H, Ung CO, Cai Y. Benefits and challenges of electronic health record system on stakeholders: a qualitative study of outpatient physicians. J Med Syst 2013;37(4):9960. https://doi.org/10.1007/s10916-013-9960-5
A10. Cifuentes M, Davis M, Fernald D, Gunn R, Dickinson P, Cohen DJ. Electronic health record challenges, workarounds, and solutions observed in practices integrating behavioral health and primary care. J Am Board Fam Med 2015;28(Suppl 1):S63-72. https://doi.org/10.3122/jabfm.2015.S1.150133
A11. de Hoop T, Neumuth T. Evaluating electronic health record limitations and time expenditure in a German medical center. Appl Clin Inform 2021;12(5):1082-90. https://doi.org/10.1055/s-0041-1739519
A12. Nimjee T, Miller E, Solomon S. Exploring generational differences in physicians’ perspectives on the proliferation of technology within the medical field: a narrative study. Healthc Q 2020;23(SP):53-9. https://doi.org/10.12927/hcq.2020.26172
A13. Gumede-Moyo S, Todd J, Bond V, Mee P, Filteau S. A qualitative inquiry into implementing an electronic health record system (SmartCare) for prevention of mother-to-child transmission data in Zambia: a retrospective study. BMJ Open 2019;9(9):e030428. https://doi.org/10.1136/bmjopen-2019-030428
A14. O’Malley AS, Draper K, Gourevitch R, Cross DA, Scholle SH. Electronic health records and support for primary care teamwork. J Am Med Inform Assoc 2015;22(2):426-34. https://doi.org/10.1093/jamia/ocu029
A15. Terry AL, Stewart M, Fortin M, Wong ST, Kennedy M, Burge F, et al. Gaps in primary healthcare electronic medical record research and knowledge: findings of a pan-Canadian study. Healthc Policy 2014;10(1):46-59. https://doi. org/10.12927/hcpol.2014.23927
A16. Aldosari B. Causes of EHR projects stalling or failing: a study of EHR projects in Saudi Arabia. Comput Biol Med 2017;91:372-81. https://doi.org/10.1016/j.compbiomed.2017.10.032
A17. Goetz Goldberg D, Kuzel AJ, Feng LB, DeShazo JP, Love LE. EHRs in primary care practices: benefits, challenges, and successful strategies. Am J Manag Care 2012;18(2):e48-54.
A18. Cracknell AN. Healthcare professionals’ attitudes of implementing a chemotherapy electronic prescribing system: a mixed methods study. J Oncol Pharm Pract 2020;26(5):1164-71. https://doi.org/10.1177/1078155219892304
A19. Sherer SA, Meyerhoefer CD, Sheinberg M, Levick D. Integrating commercial ambulatory electronic health records with hospital systems: an evolutionary process. Int J Med Inform 2015;84(9):683-93. https://doi.org/10.1016/j.ijmedinf.2015.05.010
A20. Umstead CN, Unertl KM, Lorenzi NM, Novak LL. Enabling adoption and use of new health information technology during implementation: roles and strategies for internal and external support personnel. J Am Med Inform Assoc 2021;28(7):1543-7. https://doi.org/10.1093/jamia/ocab044
A21. Bouamrane MM, Mair FS. A study of general practitioners’ perspectives on electronic medical records systems in NHSScotland. BMC Med Inform Decis Mak 2013;13:58. https://doi.org/10.1186/1472-6947-13-58
A22. Moon MC, Hills R, Demiris G. Understanding optimization processes of electronic health records (EHR) in select leading hospitals: a qualitative study. J Innov Health Inform 2018;25(2):109-25. https://doi.org/10.14236/jhi.v25i2.1011
A23. Militello LG, Arbuckle NB, Saleem JJ, Patterson E, Flanagan M, Haggstrom D, et al. Sources of variation in primary care clinical workflow: implications for the design of cognitive support. Health Informatics J 2014;20(1):35-49. https://doi.org/10.1177/1460458213476968
A24. Xiao SQ, Liu JE, Chang H. Physician-nurse communication surrounding computerized physician order entry systems from social and technical perspective: an ethnographic study. Comput Inform Nurs 2021;40(4):258-68. https://doi.org/10.1097/CIN.0000000000000809
A25. Nelson P, Bell AJ, Nathanson L, Sanchez LD, Fisher J, Anderson PD. Ethnographic analysis on the use of the electronic medical record for clinical handoff. Intern Emerg Med 2017;12(8):1265-72. https://doi.org/10.1007/s11739-016-1567-7
A26. Lanham HJ, Leykum LK, McDaniel RR Jr. Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc 2012;19(3):382-91. https://doi.org/10.1136/amiajnl-2011-000263
A27. Macabasag RA, Mallari EU, Pascual PJ, Fernandez-Marcelo PG. Normalisation of electronic medical records in routine healthcare work amidst ongoing digitalisation of the Philippine health system. Soc Sci Med 2022;307:115182. https://doi.org/10.1016/j.socscimed.2022.115182
A28. Klarenbeek SE, Schuurbiers-Siebers OC, van den Heuvel MM, Prokop M, Tummers M. Barriers and facilitators for implementation of a computerized clinical decision support system in lung cancer multidisciplinary team meetings: a qualitative assessment. Biology (Basel) 2020;10(1):9. https://doi.org/10.3390/biology10010009
A29. Bergey MR, Goldsack JC, Robinson EJ. Invisible work and changing roles: health information technology implementation and reorganization of work practices for the inpatient nursing team. Soc Sci Med 2019;235:112387. https://doi.org/10.1016/j.socscimed.2019.112387
A30. Pontefract SK, Coleman JJ, Vallance HK, Hirsch CA, Shah S, Marriott JF, et al. The impact of computerised physician order entry and clinical decision support on pharmacist-physician communication in the hospital setting: a qualitative study. PLoS One 2018;13(11):e0207450. https://doi.org/10.1371/journal.pone.0207450
A31. Grando MA, Vellore V, Duncan BJ, Kaufman DR, Furniss SK, Doebbeling BN, et al. Study of EHR-mediated workflows using ethnography and process mining methods. Health Informatics J 2021;27(2):14604582211008210. https://doi.org/10.1177/14604582211008210
A32. Prater L, Sanchez A, Modan G, Burgess J, Frier K, Richards N, et al. Electronic health record documentation patterns of recorded primary care visits focused on complex communication: a qualitative study. Appl Clin Inform 2019;10(2):247- 53. https://doi.org/10.1055/s-0039-1683986
A33. Howard J, Clark EC, Friedman A, Crosson JC, Pellerano M, Crabtree BF, et al. Electronic health record impact on work burden in small, unaffiliated, community-based primary care practices. J Gen Intern Med 2013;28(1):107-13. https://doi.org/10.1007/s11606-012-2192-4
A34. Friedman A, Crosson JC, Howard J, Clark EC, Pellerano M, Karsh BT, et al. A typology of electronic health record workarounds in small-to-medium size primary care practices. J Am Med Inform Assoc 2014;21(e1):e78-83. https://doi. org/10.1136/amiajnl-2013-001686
A35. Bar-Lev S. The politics of healthcare informatics: knowledge management using an electronic medical record system. Sociol Health Illn 2015;37(3):404-21. https://doi.org/10.1111/1467-9566.12213
A36. Boonstra A, Jonker TL, van Offenbeek MA, Vos JF. Persisting workarounds in Electronic Health Record System use: types, risks and benefits. BMC Med Inform Decis Mak 2021;21(1):183. https://doi.org/10.1186/s12911-021-01548-0
A37. Chao CA. The impact of electronic health records on collaborative work routines: a narrative network analysis. Int J Med Inform 2016;94:100-11. https://doi.org/10.1016/j.ijmedinf.2016.06.019
A38. Acharya A, Shimpi N, Mahnke A, Mathias R, Ye Z. Medical care providers’ perspectives on dental information needs in electronic health records. J Am Dent Assoc 2017;148(5):328-37. https://doi.org/10.1016/j.adaj.2017.01.026
A39. Rudin RS, Fischer SH, Damberg CL, Shi Y, Shekelle PG, Xenakis L, et al. Optimizing health IT to improve health system performance: a work in progress. Healthc (Amst) 2020;8(4):100483. https://doi.org/10.1016/j.hjdsi.2020.100483
A40. Tran BD, Rosenbaum K, Zheng K. An interview study with medical scribes on how their work may alleviate clinician burnout through delegated health IT tasks. J Am Med Inform Assoc 2021;28(5):907-14. https://doi.org/10.1093/jamia/ocaa345
A41. Soriano R, Siegel EO, Kim TY, Catz S. Nurse managers’ experiences with electronic health records in quality monitoring. Nurs Adm Q 2019;43(3):222-9. https://doi.org/10.1097/NAQ.0000000000000352
A42. Despins LA, Wakefield BJ. The role of the electronic medical record in the intensive care unit nurse’s detection of patient deterioration: a qualitative study. Comput Inform Nurs 2018;36(6):284-92. https://doi.org/10.1097/CIN.0000000000000431
A43. Staggers N, Clark L, Blaz JW, Kapsandoy S. Nurses’ information management and use of electronic tools during acute care handoffs. West J Nurs Res 2012;34(2):153-73. https://doi.org/10.1177/0193945911407089
A44. Ozkaynak M, Reeder B, Drake C, Ferrarone P, Trautner B, Wald H. Characterizing workflow to inform clinical decision support systems in nursing homes. Gerontologist 2019;59(6):1024-33. https://doi.org/10.1093/geront/gny100
A45. Abbott AA, Fuji KT, Galt KA. A qualitative case study exploring nurse engagement with electronic health records and E-prescribing. West J Nurs Res 2015;37(7):935-51. https://doi.org/10.1177/0193945914567359
A46. Zhao JY, Kessler EG, Guo WA. Interprofessional communication goes up when the electronic health record goes down. J Surg Educ 2019;76(2):512-8. https://doi.org/10.1016/j.jsurg.2018.08.024
A47. Moerenhout T, Fischer GS, Saelaert M, De Sutter A, Provoost V, Devisch I. Primary care physicians’ perspectives on the ethical impact of the electronic medical record. J Am Board Fam Med 2020;33(1):106-17. https://doi.org/10.3122/jabfm.2020.01.190154
A48. Jensen LG, Bossen C. Factors affecting physicians’ use of a dedicated overview interface in an electronic health record: the importance of standard information and standard documentation. Int J Med Inform 2016;87:44-53. https://doi.org/10.1016/j.ijmedinf.2015.12.009
A49. Schweitzer M, Lasierra N, Hoerbst A. Requirements for Workflow-Based EHR Systems: Results of a Qualitative Study. Stud Health Technol Inform 2016;223:124-31.
A50. Patel VL, Denton CA, Soni HC, Kannampallil TG, Traub SJ, Shapiro JS. Physician workflow in two distinctive emergency departments: an observational study. Appl Clin Inform 2021;12(1):141-52. https://doi.org/10.1055/s-0040-1722615
A51. Denton CA, Soni HC, Kannampallil TG, Serrichio A, Shapiro JS, Traub SJ, et al. Emergency physicians’ perceived influence of EHR use on clinical workflow and performance metrics. Appl Clin Inform 2018;9(3):725-33. https://doi.org/10.1055/s-0038-1668553
A52. Quinn M, Forman J, Harrod M, Winter S, Fowler KE, Krein SL, et al. Electronic health records, communication, and data sharing: challenges and opportunities for improving the diagnostic process. Diagnosis (Berl) 2019;6(3):241-8. https://doi.org/10.1515/dx-2018-0036
A53. Lanham HJ, Sittig DF, Leykum LK, Parchman ML, Pugh JA, McDaniel RR. Understanding differences in electronic health record (EHR) use: linking individual physicians’ perceptions of uncertainty and EHR use patterns in ambulatory care. J Am Med Inform Assoc 2014;21(1):73-81. https://doi.org/10.1136/amiajnl-2012-001377
A54. Ash JS, Sittig DF, McMullen CK, Wright A, Bunce A, Mohan V, et al. Multiple perspectives on clinical decision support: a qualitative study of fifteen clinical and vendor organizations. BMC Med Inform Decis Mak 2015;15:35. https://doi.org/10.1186/s12911-015-0156-4
A55. Olayiwola JN, Rubin A, Slomoff T, Woldeyesus T, Willard-Grace R. Strategies for Primary Care Stakeholders to Improve Electronic Health Records (EHRs). J Am Board Fam Med 2016;29(1):126-34. https://doi.org/10.3122/jabfm.2016.01.150212
A56. Hollin I, Griffin M, Kachnowski S. How will we know if it’s working?: a multi-faceted approach to measuring usability of a specialty-specific electronic medical record. Health Informatics J 2012;18(3):219-32. https://doi.org/10.1177/1460458212437008
A57. Mozaffar H, Williams R, Cresswell K, Morrison Z, Bates DW, Sheikh A. The evolution of the market for commercial computerized physician order entry and computerized decision support systems for prescribing. J Am Med Inform Assoc 2016;23(2):349-55. https://doi.org/10.1093/jamia/ocv095
A58. Cresswell KM, Lee L, Slee A, Coleman J, Bates DW, Sheikh A. Qualitative analysis of vendor discussions on the procurement of Computerised Physician Order Entry and Clinical Decision Support systems in hospitals. BMJ Open 2015;5(10):e008313. https://doi.org/10.1136/bmjopen-2015-008313
A59. Cohen DJ, Wyte-Lake T, Dorr DA, Gold R, Holden RJ, Koopman RJ, et al. Unmet information needs of clinical teams delivering care to complex patients and design strategies to address those needs. J Am Med Inform Assoc 2020;27(5):690-9. https://doi.org/10.1093/jamia/ocaa010
A60. Sicotte C, Clavel S, Fortin MA. A cancer care electronic medical record highly integrated into clinicians’ workflow: users’ attitudes pre-post implementation. Eur J Cancer Care (Engl) 2017;26(6):e12548. https://doi.org/10.1111/ecc.12548
A61. Rathert C, Porter TH, Mittler JN, Fleig-Palmer M. Seven years after meaningful use: physicians’ and nurses’ experiences with electronic health records. Health Care Manage Rev 2019;44(1):30-40. https://doi.org/10.1097/HMR.0000000000000168
A62. Gonzalez Z, Recondo F, Sommer J, Schachner B, Garcia G, Luna D, et al. Nurses’ expectations and perceptions of a redesigned electronic health record. Stud Health Technol Inform 2015;210:374-8. https://doi.org/10.3233/978-1-61499-512-8-374
A63. Zadvinskis IM, Chipps E, Yen PY. Exploring nurses’ confirmed expectations regarding health IT: a phenomenological study. Int J Med Inform 2014;83(2):89-98. https://doi.org/10.1016/j.ijmedinf.2013.11.001
A64. Wisner K, Chesla CA, Spetz J, Lyndon A. Managing the tension between caring and charting: labor and delivery nurses’ experiences of the electronic health record. Res Nurs Health 2021;44(5):822-32. https://doi.org/10.1002/nur.22177
A65. Holden RJ. Social and personal normative influences on healthcare professionals to use information technology: towards a more robust social ergonomics. Theor Issues Ergon Sci 2012;13(5):546-69. https://doi.org/10.1080/1463922X.2010.549249
A66. Al Alawi S, Al Dhaheri A, Al Baloushi D, Al Dhaheri M, Prinsloo EA. Physician user satisfaction with an electronic medical records system in primary healthcare centres in Al Ain: a qualitative study. BMJ Open 2014;4(11):e005569. https://doi.org/10.1136/bmjopen-2014-005569
A67. Terry AL, Ryan BL, McKay S, Oates M, Strong J, McRobert K, et al. Towards optimal electronic medical record use: perspectives of advanced users. Fam Pract 2018;35(5):607-11. https://doi.org/10.1093/fampra/cmy002
A68. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag 2016;13(Winter):1d.
A69. Hobensack M, Ojo M, Bowles K, McDonald M, Song J, Topaz M. Home healthcare clinicians’ perspectives on electronic health records: a qualitative study. Stud Health Technol Inform 2021;284:426-30. https://doi.org/10.3233/SHTI210763
A70. Abramson EL, Patel V, Malhotra S, Pfoh ER, Nena Osorio S, Cheriff A, et al. Physician experiences transitioning between an older versus newer electronic health record for electronic prescribing. Int J Med Inform 2012;81(8):539-48. https://doi.org/10.1016/j.ijmedinf.2012.02.010
A71. Westerbeek L, de Bruijn GJ, van Weert HC, Abu-Hanna A, Medlock S, van Weert JC. General Practitioners’ needs and wishes for clinical decision support Systems: a focus group study. Int J Med Inform 2022;168:104901. https://doi.org/10.1016/j.ijmedinf.2022.104901
A72. Halas G, Singer A, Styles C, Katz A. New conceptual model of EMR implementation in interprofessional academic family medicine clinics. Can Fam Physician 2015;61(5):e232-9.
A73. Sheikh A, Sood HS, Bates DW. Leveraging health information technology to achieve the “triple aim” of healthcare reform. J Am Med Inform Assoc 2015;22(4):849-56. https://doi.org/10.1093/jamia/ocv022
A74. Koutzampasopoulou Xanthidou O, Shuib L, Xanthidis D, Nicholas D. Electronic medical records in Greece and Oman: a professional’s evaluation of structure and value. Int J Environ Res Public Health 2018;15(6):1137. https://doi.org/10.3390/ijerph15061137