Healthcare Information Technology: A Systematic Mapping Study
Article information
Abstract
Objectives
This paper presents a systematic mapping of studies related to information systems and technology in the field of healthcare, enabling a visual mapping of the different lines of knowledge that can provide an overview of the scientific literature in this field. This map can help to clarify critical aspects of healthcare informatics, such as the main types of information systems, the ways in which they integrate with each other, and the technological trends in this field.
Methods
Systematic mapping refers to a process of classifying information in a given area of knowledge. It provides an overview of the state of the art in a particular discipline or area of knowledge, establishing a map that describes how knowledge is structured in that particular area. In this study, we proposed and carried out a specific implementation of the methodology for mapping. In total, 1,619 studies that combine knowledge related to information systems, computer science, and healthcare were selected and compiled from prestigious publications.
Results
The results established a distribution of the available literature and identified papers related to certain research questions, thereby providing a map of knowledge that structures the different trends and main areas of research, making it possible to address the research questions and serving as a guide to deepen specific aspects of the field of study.
Conclusions
We project and propose future research for the trends that stand out because of their interest and the possibility of exploring these topics in greater depth.
I. Introduction
Healthcare and its improvement have historically been one of the highest priorities both individually and for society [1]. Several factors improve both the length and quality of life, among which one of the most important is the quality of healthcare and clinical care [2]. In this context, information technology has emerged as a tool that helps healthcare both quantitatively and qualitatively [3]. The primary purpose of information technology in healthcare is to automate and facilitate tasks previously carried out manually, with examples including the digitization of health records, job listings, clinical records, and paper requests for clinical tests [4].
The management of clinical information systems became a profession with the emergence of real enterprise resource planning solutions or global business management systems (hospital information systems), and also with the treatment of clinical data (clinical information systems) [5]. Simultaneously, technology has been increasingly used in clinical practice to perform new tasks or obtain information that would have been otherwise unworkable or directly impossible. Clinical analysis tools and support systems for surgical interventions are good examples of this [6]. Ongoing technological progress and new developments constitute a considerable source of innovation that can result in substantial improvements for healthcare systems. Relatively recent concepts such as big data [7], telemedicine [8], and the Internet of Things (IoT) [9] are already part of everyday life in healthcare settings.
Globalization is, in our opinion, one of the most significant challenges that information technology faces in the field of healthcare. Interoperability between systems and the need for the homogenization of processes and information among different agents demand robust criteria to make decisions [10]. Standards are the result of the work of organizations focused on structuring clinical information and the means for communicating and interpreting it. A common standardized language is a fundamental prerequisite for the implementation of new technologies encompassing organizations globally [11].
In order to address the application of technology in the healthcare field, it is essential to be familiar with the knowledge provided by previous research to avoid redundant work and to avoid making mistakes that are already known. For this reason, systematic research on previous publications allows us to obtain a global vision of this field of knowledge.
This paper presents a systematic mapping of the state-of-the-art of information systems in the field of healthcare to characterize the different trends of information technologies in the healthcare field, raised as research questions (RQs). The next section describes the methodology used.
II. Methods
Systematic mapping is a process of classifying information in a particular area of knowledge. It yields an overview of the state of the art in a particular discipline or area of knowledge, establishing a visual map that describes how knowledge in that particular area is structured, as stated by Barbosa and Alves [12]. Systematic mapping is a technique related to systematic literature reviews, although systematic mapping does not provide information on the depth of the published literature at the same level that a systematic literature review enables. However, systematic mapping may be a better choice as an initial approach to determine the level of progress in particular fields or areas, which can then be followed by a systematic review of the literature if needed.
In our particular case, when facing a field as broad as information systems in healthcare, the first approach should be conducted using systematic mapping.
Although we did not use a specific protocol to conduct the systematic mapping, we followed the methodology of systematic mapping presented by Petersen et al. [13], applying several criteria for classification and mapping as suggested by Engstrom and Runeson [14], and adapting the methodology to the specific aspects of the field of study. The steps of systematic mapping are as follows: (1) reviewing the scope, (2) conducting the search, (3) gathering all papers, (4) screening the papers, (5) assessing the impact of primary keywords, (6) developing a classification scheme, (7) assessing the impact of secondary keywords, and (8) conducting data extraction and the mapping process.
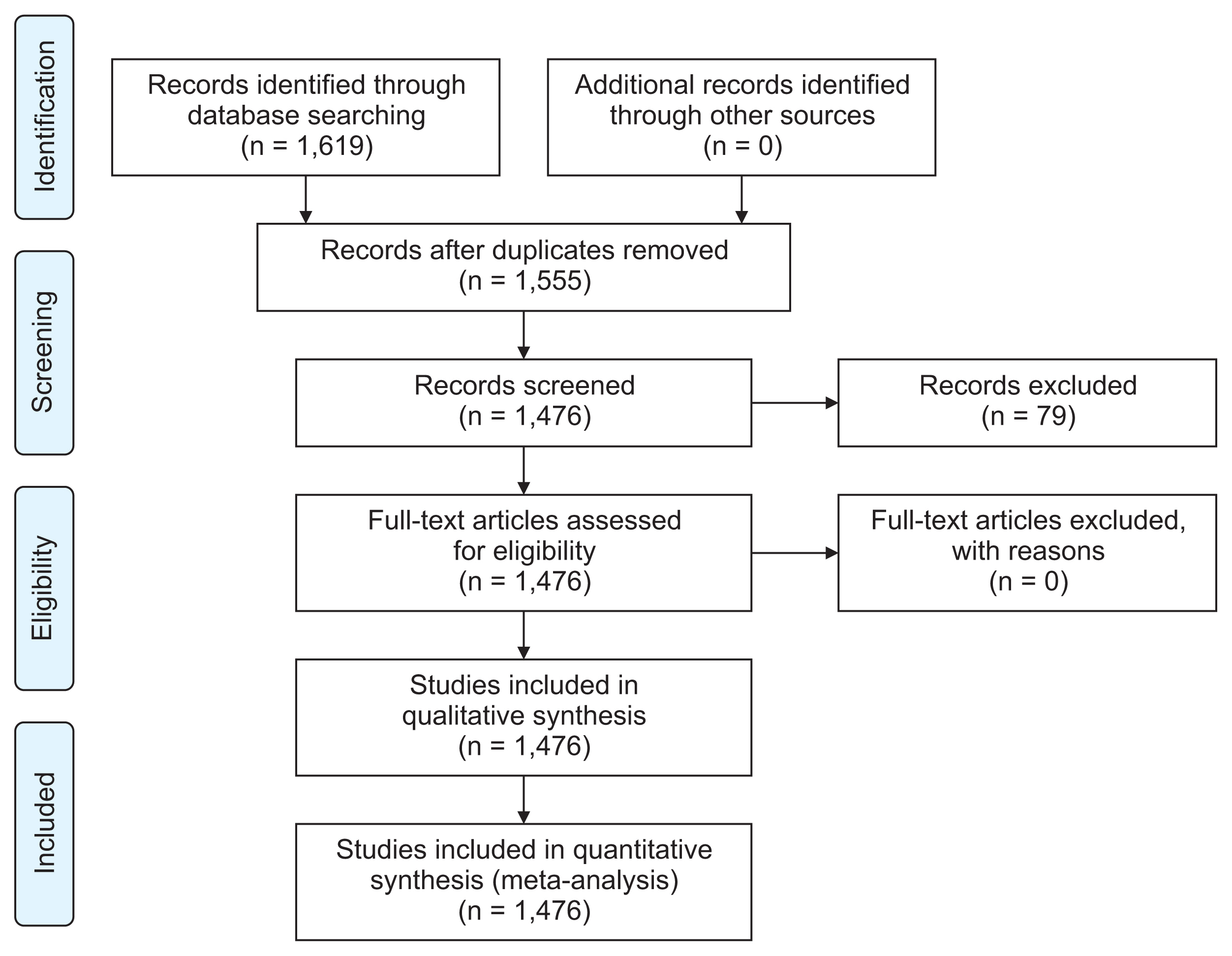
The volume of records processed was described according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standard [15], as shown in Figure 1.
Systematic mappings usually tend to cover narrower areas of knowledge. The generality of the area studied allows for a complete overview of the scope of the area, but also presents as a constraint the impossibility of dealing in depth with specific aspects, which should be left for later studies.
1. Definition of Research Questions
This study set out to address the following RQs dealing with information systems within the field of healthcare:
RQ1: What technological solutions are used as clinical information systems and for healthcare management?
RQ2: How are those information systems integrated?
RQ3: What are the technological trends in the healthcare field?
2. Review Scope
The data sources were repositories whose areas of knowledge included technology. The results of the systematic mapping should identify which sources are more specialized in information systems as related to healthcare.
The selected sources were ACM Digital Library (ACM), IEEEXplore (IEEEX), Google Scholar (GS), ISI Web of Knowledge (WoK), CiteSeerX (CSX), Science Direct (SD), Springer (SL), The Collection of Computer Science Bibliographies (CSB), Scopus (SCO), ResearchGate (RG), PLOS One (PO), PubMed (PM).
The search period had no initial date, and it included studies until December 2017.
3. Conduct Search
(1) Search terms were selected according to the following premises:
(2) Papers should be technical, and related to technology and information systems.
(3) The area in which each paper is framed should be healthcare.
(4) Papers should deal with at least one of the leading areas of knowledge from which a taxonomy can be established: architecture, integration, and standards.
(5) Synonyms or similar terms should be considered.
The quality of the paper was not quantified or assessed.
The contribution, significance, or other scientific merits were not used to discard papers. The objective was to map the current situation of literature in the given area. It was not to select high-quality papers.
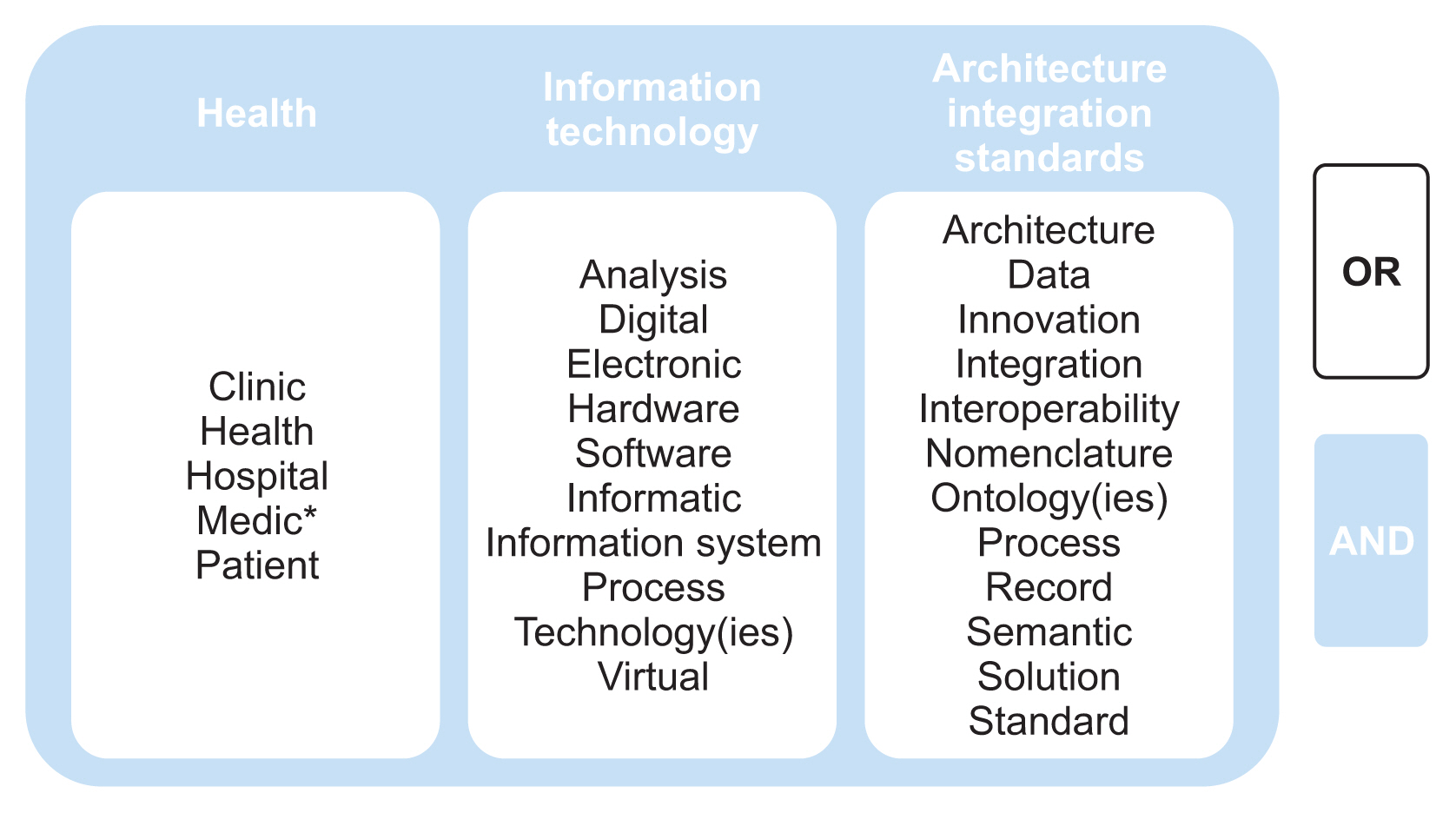
Based on these criteria, we selected three sets of search terms: (1) terms relating to health, (2) terms relating to information technology, and (3) terms relating to architecture, integration, and standards.
The selected terms, called “primary keywords,” are shown in Figure 2.
Broader terms were not taken into account to avoid redundancies (e.g., “Electronic Device” when “Electronic” is already taken into account). The following search query was used: (“Clinic” OR “Health” OR “Hospital” OR “Medic*” OR “Patient”) AND (“Analysis” OR “Digital” OR “Electronic” OR “Hardware” OR “Software” OR “Information System” OR “Process” OR “Informatic” OR “Technology” OR “Technologies” OR “Virtual”) AND (“Architecture” OR “Data” OR “Innovation” OR “Integration” OR “Interoperability” OR “Nomenclature” OR “Ontology” OR “Ontologies” OR “Record” OR “Semantic” OR “Solution” OR “Standard”).
4. Gathering All Papers
The heterogeneity of the data sources makes it necessary to make adjustments in the search string and filtering criteria (mainly by the paper title) to locate candidate studies that are relevant.
The number of papers obtained for each source was as follows: ACM (59), IEEEX (31), GS (86), WoK (284), CSX (239), SD (29), SL (165), CSB (532), SCO (75), RG (48), PO (16), and PM (55). In total, 1,619 papers were obtained.
5. Screening of Papers
The obtained studies were reviewed, removing duplicates and papers whose topic or content was unrelated to the subject of the investigation.
After removing the studies that were duplicates (64) or irrelevant (79), the number of studies considered for the elaboration of the map was 1,476.
6. Impact of Primary Keywords
An analysis of the 1,476 resulting studies was carried out, quantifying the occurrence of the different keywords in each of them. For this purpose, the information on the 1,476 studies was registered in a database, and a customized computer application was designed and implemented to process the information about the studies.
We then quantified the occurrence of each keyword. To indicate the relevance of each word, we used the Fibonacci series, where growth was represented through an exponential ratio in order to maintain the proportions that keep the readability of the results, as indicated by Basak [16]. More specifically, we applied the formula F(n) = F(n–2) + F(n−1) and assigned a value ranging from 1 to 10 that represented the relevance of each keyword based on the minimum number of occurrences according to the Fibonacci series, starting with the eighth value of 21. Therefore, a keyword was considered to be of relevance 1 if its number of occurrences was less than or equal to 21 (F(8)), of relevance 2 if it was between 21 and 34 (F(9)), of relevance 3 if it was between 34 and 55 (F(10)), and so forth, up to a relevance of 8 it had between 377 (F(15)) and 610 (F(16)) occurrences. We then obtained the distribution of relevance for the different keywords analyzed, as shown in Table 1.
We also carried out an analysis between each pair of keywords to determine the frequency of their co-occurrence in the selected articles, as presented in Figure 3. In this way, we analyze the correlation of each keyword with the rest, in order to assess the relative relevance of each term.
7. Classification Scheme
After taking into consideration the relevance of the different keywords, their relationships with each other in the papers, and a selection of technological terms applied to health contexts, we selected secondary keywords from the highest-impact papers. Secondary keywords facilitate assessing the volume of publications of different subtopics. The list of secondary keywords is presented in Figure 4.
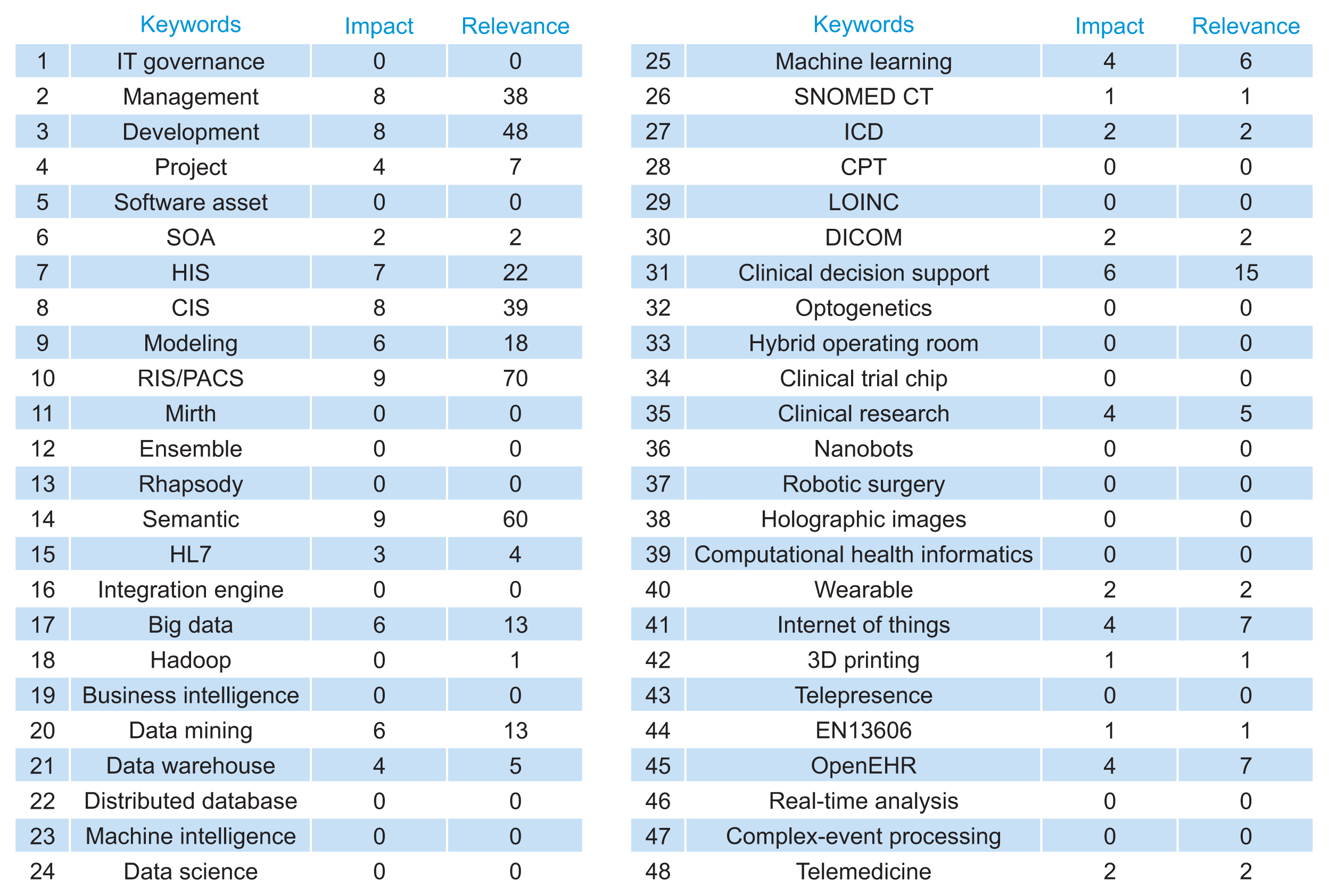
Comparison of relevant results for secondary keywords. IT: information technology, SOA: service-oriented architecture, HIS: health information system, CIS: clinical information system, RIS: radiology information system, PACS: picture archiving and communication system, ICD: International Classification of Diseases, EHR: Electronic Health Record, CPT: Current Procedural Terminology, LOINC: Logical Observation Identifiers Names and Codes, DICOM: Digital Imaging and Communications in Medicine, HL7: Health Level 7.
8. Impact of Secondary Keywords
We analyzed secondary keywords in the same way that we did with the primary keywords. We used the impact analysis application and the list of publications to compute the occurrence of secondary keywords in the 1,476 articles selected after removing duplicate and irrelevant articles. The occurrence of each keyword was quantified, and a value ranging from 1 to 10 was assigned to the relevance of each keyword based on the minimum number of occurrences, following the Fibonacci series, as was done with the primary keywords.
The results obtained are presented in Figure 4, showing the correspondence of the impact level for each of the secondary keywords. We also analyzed the co-occurrence of keywords (Figures 5, 6). The value “0” indicates no matches. The figures presenting co-occurrence are separated into two parts (block I and block II) to increase readability. The indices in the first row and first column refer to the numbered terms in Figure 4.
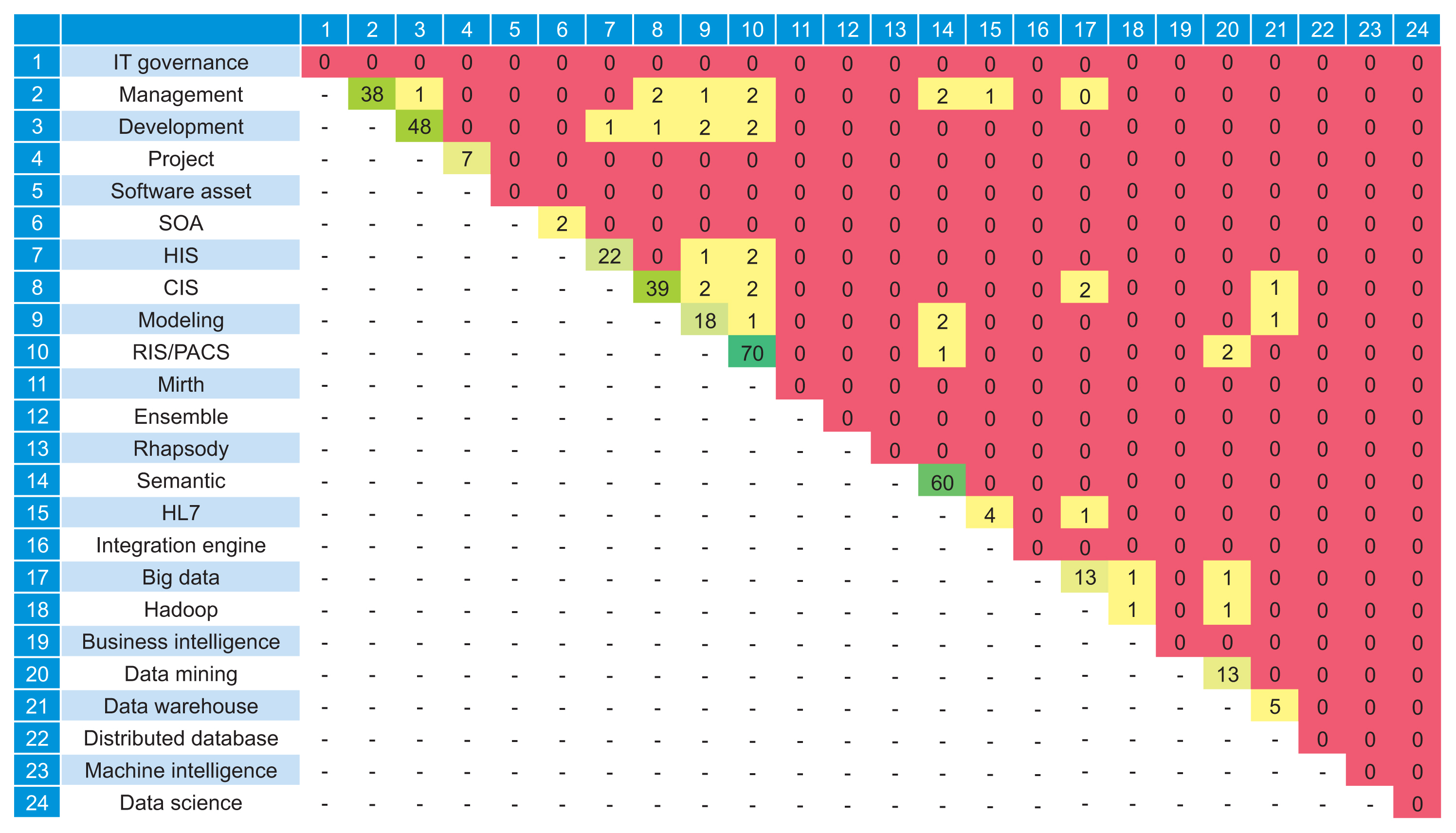
Analysis of the co-occurrence of secondary keywords (block I). IT: information technology, SOA: service-oriented architecture, HIS: health information system, CIS: clinical information system, RIS: radiology information system, PACS: picture archiving and communication system, HL7: Health Level 7.

Analysis of the co-occurrence of secondary keywords (block II). IT: information technology, SOA: service-oriented architecture, HIS: health information system, CIS: clinical information system, RIS: radiology information system, PACS: picture archiving and communication system, HL7: Health Level 7, ICD: International Classification of Diseases, CPT: Current Procedural Terminology, LOINC: Logical Observation Identifiers Names and Codes, DICOM: Digital Imaging and Communications in Medicine, EHR: Electronic Health Record.
A longitudinal analysis of the keywords was carried out to show the tendencies in the frequency of keywords over time. To do this, we analyzed the number of occurrences of each keyword in the datasets of the selected studies annually, as shown in Figure 7.
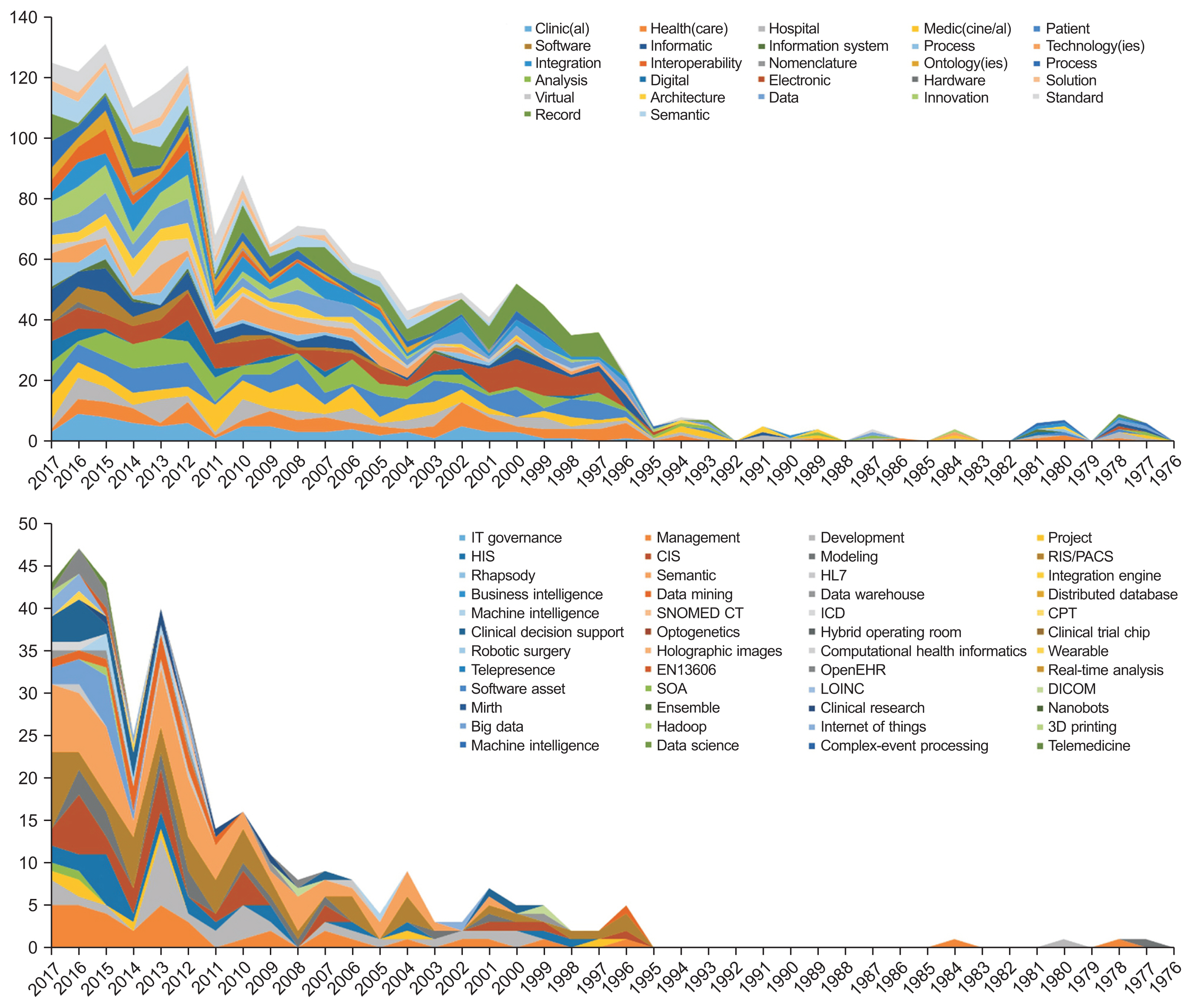
Historical trends in the keywords. IT: information technology, HIS: health information system, CIS: clinical information system, SOA: service-oriented architecture, HL7: Health Level 7, ICD: International Classification of Diseases, EHR: Electronic Health Record, LOINC: Logical Observation Identifiers Names and Codes, RIS: radiology information system, PACS: picture archiving and communication system, CPT: Current Procedural Terminology, DICOM: Digital Imaging and Communications in Medicine.
9. Data Extraction and Mapping Process
The mapping of the selected relevant studies was conducted by quantifying the occurrences of keywords and their relationships, establishing a classification of all papers in one or more of the defined categories. In this way, based on the incidence of specific terms or concepts that identify an area of knowledge within the scope of the investigation, we could quantify the actual volume of studies related to each of these areas. The results are presented graphically in Figure 8.
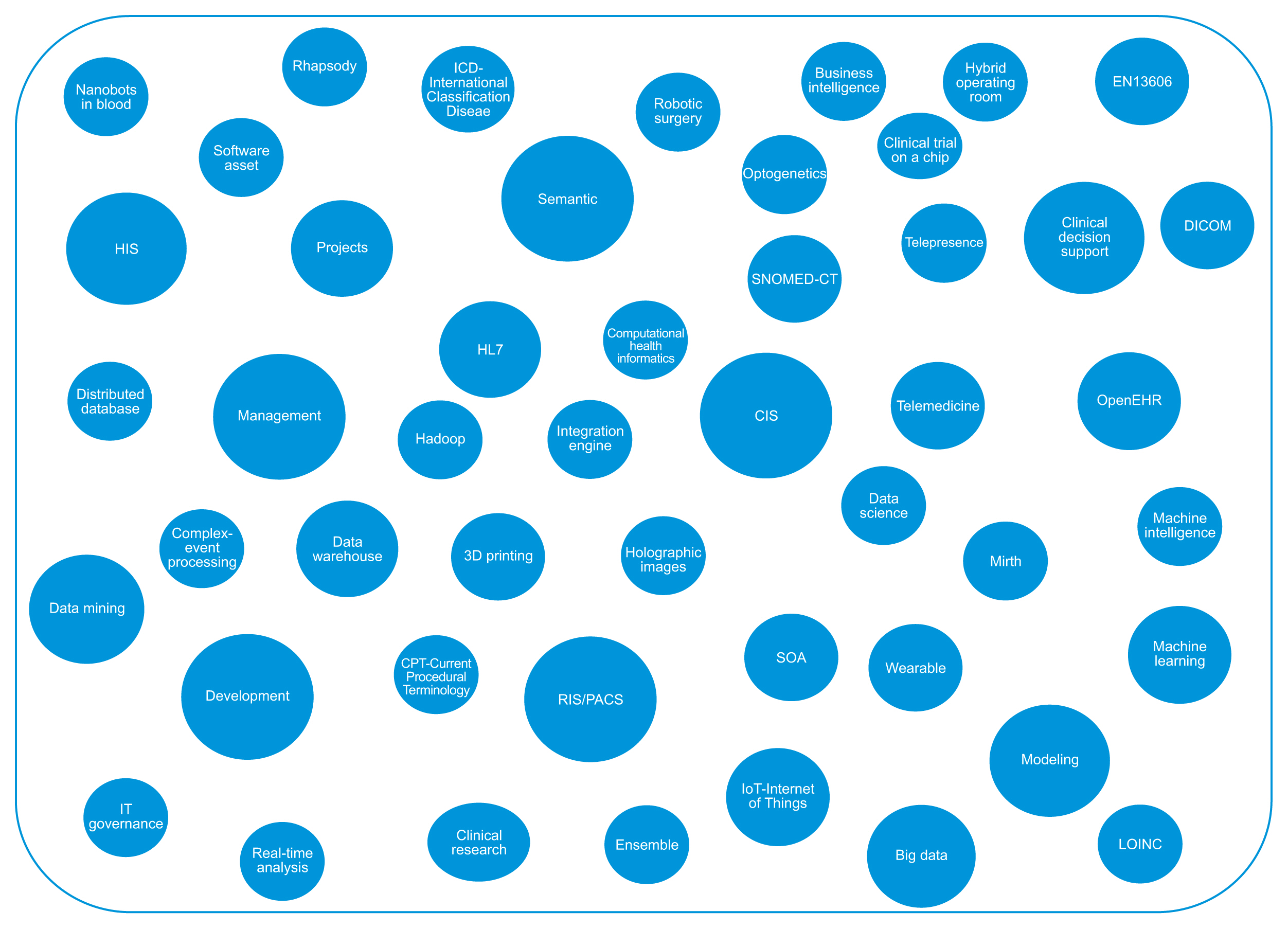
Set of secondary keywords according to their relevance. SOA: service-oriented architecture, HIS: health information system, CIS: clinical information system, RIS: radiology information system, PACS: picture archiving and communication system, ICD: International Classification of Diseases, EHR: Electronic Health Record, LOINC: Logical Observation Identifiers Names and Codes, DICOM: Digital Imaging and Communications in Medicine, HL7: Health Level 7.
III. Results
After processing all the information using the systematic mapping methodology with all the extracted data, sufficient information was available to group and visualize the structure of the information. For this purpose, the secondary keywords were grouped by topics, and considering the relevance of the terms and their co-occurrence patterns, the map of technologies and information systems is presented in Figure 9.
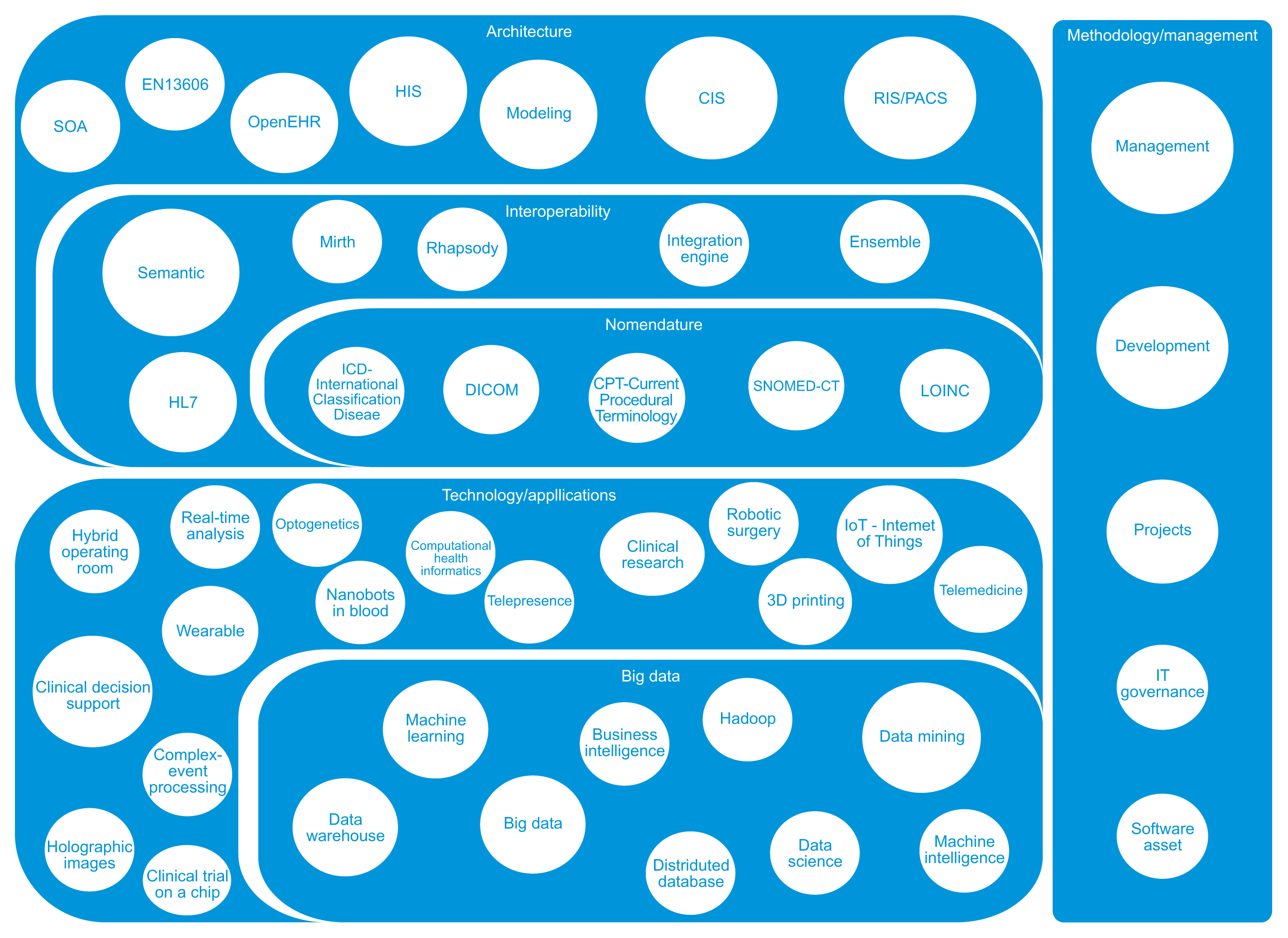
Map of technologies and information systems. SOA: service-oriented architecture, HIS: health information system, CIS: clinical information system, RIS: radiology information system, PACS: picture archiving and communication system, EHR: Electronic Health Record, LOINC: Logical Observation Identifiers Names and Codes, DICOM: Digital Imaging and Communications in Medicine, HL7: Health Level 7.
Obtaining the map of technologies and information systems will make it possible to address the RQs. Specifically, of the 1,476 papers, 238 dealt with solution-related topics, 120 with integration, and 77 with technology trends.
Carrying out systematic mapping made it possible to classify and analyze the situation of healthcare information systems and technologies from a neutral point of view. In light of the systematic mapping and the studies analyzed, we now address the research questions.
-RQ1: What technological solutions are used as clinical information systems and healthcare management?
In the map of technologies and information systems, we can see a clear differentiation between the methodology and management category and the architecture solutions, which cover the operational needs of clinical registries. Clinical information systems aim to handle clinical information, which can be divided into clinical data and clinical operative management data. In complex healthcare environments, such as large clinical centers, it is necessary to combine different specialized solutions to meet the needs of information management. Not surprisingly, the largest and most complex solutions have been the most frequently studied and analyzed. These solutions emphasize hospital information management systems [17], clinical information systems [18], radiological information management systems with storage and communication capabilities [19], and laboratory information systems [20]. These tools have been analyzed from different perspectives including, the functional point of view, the technical structure, the software architecture, and the success of their deployment. In practice, there are multiple solutions, both open source and proprietary, and even custom solutions. Additionally, many clinical information systems with specific purposes are available to support very particular needs, such as care for patients in a particular clinical specialty. These systems cover the organization's operational workflow, and they can produce reports and statistics from specific data. These systems usually rely on the large solutions previously mentioned [21].
-RQ2: How are these information systems integrated?
As indicated in RQ1, we found several central information systems (hospital information management systems, clinical information systems, radiological information management systems with storage and communication capabilities, and laboratory information systems, as well as other dependent secondary information systems). In practice, all systems share the same core data. The patient is at the center of the information, mainly in the form of electronic health records [22–24]. In a critical operating environment, such as a clinical care organization, it is essential to maintain principles such as data coherence and efficiency in information management. For this reason, interoperability between systems is probably the most critical factor in the implementation and management of an information system [25], both regarding communication [26] and the semantic interpretation of information [27].
We can see in the map how, in addition to covering traditional interoperability aspects, semantic standardization and nomenclature aspects are increasingly covered.
As solutions for integration, simpler mechanisms such as web services or sharing database tables exist. However, in minimally complex environments, the solution most commonly adopted is the use of integration engines. Integration engines are an efficient, structured, adaptive and multi-platform mechanism for information exchange that enables multiple messages to be sent sequentially among multiple points [28]. The adoption of standards also facilitates interoperability among heterogeneous information systems [29]. HL7 [30] is the primary protocol for information exchange, while naming standards like SNOMED-CT [31], ICD [32] and DICOM [33] are used for information encoding.
-RQ3: What are the technological trends in the healthcare field?
Continuing technological advances in the clinical field provide compelling possibilities for improving solutions to existing problems, as well as new ways to face challenges that were not even considered problems. With regard to new technologies, the map shows great heterogeneity, although several of the possible trends may end up being of marginal relevance. The rise of technologies that maximize the use of big data does seem clear. The historical evolution of the secondary keywords shows that support for clinical decision-making is an example of this and that it is now one of the leading fields of study. Support for clinical decision-making facilitates processing vast amounts of information using heuristics to obtain results unachievable exclusively through human intervention [34]. Other trends are the use of wearable devices [35] and the IoT [36], advances in clinical research and 3D printing, and the surgical use of robots or hybrid operating rooms.
However, big data is the area where the most research efforts are currently being invested. The continuing increases in processing power, storage capacity, the use of information standards, and agreements between different data providers are factors that contribute to the growth of big data in healthcare environments. Thus, there is the possibility of accessing heterogeneous and distributed clinical information to obtain patterns that make it possible to address existing problems, as well as anticipating and preventing their origin [37].
IV. Discussion
It is necessary to consider the limitations inherent to systematic mapping, especially in a field as broad as this one: the number of studies considered is very large and diverse, and therefore the trends and lines of work identified in the conclusions have sufficient relevance to warrant greater depth in future studies. However, we have sufficient information to analyze previous research achievements.
The results for RQ1 suggest that a significant number of studies and efforts are related to information system architecture and specific standards and technologies. This is reasonable, as these topics constitute the foundation on which all other aspects of healthcare technology are based—in fact, they are so important that it may be necessary to adapt the rest of the healthcare environment to optimize their implementation, as indicated by Ilin et al. [38].
We can see in RQ2 that a challenge faced by complex clinical information systems is often addressed—namely, the integration of the analyzed models from a global point of view. We agree with the trend toward the use of standards for electronic health record integration, as indicated by Lin et al. [39]. In this sense, we consider there to be room for work on interoperability solutions. Research on this topic should cover healthcare organizations’ integration needs, with the goal of addressing the problems inherent to integration (complexity, standardization, heterogeneous terminologies, legacy systems, and resistance to change) raised by Iroju et al. [40].
In RQ3, we see several possible lines of research: management and governance of information systems, management of technology-driven healthcare processes, semantic interoperability of healthcare environments, and data science topics (big data or artificial intelligence). However, with the continuing evolution and improvement of technology and its impact on the environment, it is difficult to foresee long-term needs in information technologies and systems. A highly disruptive technological innovation may be enough to bring about a paradigm shift that completely alters the status quo, providing solutions that force us to rethink the issues raised. As Thimbleby [41] already stated, it is essential to review and analyze technological evolution, since doing so is the basis for finding the best solutions.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.